Less is More
Getting needed images with less ionizing radiation.
©romaset / stock.adobe.com

Atomic Age movies of the 1950s—such as Them!, Godzilla, and The Beast From 20,000 Fathoms—played on a growing trend of radiophobia (the fear of ionizing radiation), which stemmed from nuclear weapons testing and the development of nuclear energy.1
Although these movies were hyperbolic expressions of ionizing radiation’s ill effects for the sake of entertainment, they were all based on real-life concerns. Dr Otto Walkhoff—the pioneer who took the first dental radiograph—noticed hair loss in some of his patients.2 Physicist Marie Curie—the preeminent pioneer in radioactivity research—died from aplastic anemia in 1934.
No dentist wants to bombard patients with excess radiation. Precautions are taken to ensure that minimal radiation is used and innovators continually strive to lessen the amount necessary.
The Trade-Off
The good news is that clinicians do not have to use a large amount of ionizing radiation for imaging. However, more image detail is achieved with higher levels of radiation.
“Unfortunately, the downsides historically have been lower image quality,” says Brent Garvin, senior product manager of imaging for Hoffman Estates, Illinois–based Planmeca USA, a manufacturer of dental equipment. “So, if you can increase radiation, then you have better image quality.”
Radiological imaging doesn’t have to be used. Dentists can use other modern technologies to examine patients.
“The lowest radiation really comes from the old-fashioned way,” says Rob Gochoel, vice president of sales for San Jose, California–based PreXion, which manufactures dental imaging equipment. “It would be, basically, zero radiation, which would be an intraoral exam. That would be your lowest type of radiation. An intraoral camera might pick up some things and that would obviously have no radiation.”
But as imaging becomes more detailed, more radiation must be introduced. “Your lowest radiation will come from sensor-type bitewings,” Gochoel says. “And then panoramics would be a little bit more than that. Cephalometric IMS imagery would also have very low radiation overall. So, as you step up, as you get more detail in the scan, the radiation level goes higher.”
Technique
How the clinical team obtains an image helps determine the dose of radiation used. This usually starts with what the doctor prescribes, Garvin notes.
“The team member needs to work in tandem with the clinician because they are the ones who prescribe the x-ray,” Garvin says. “The team member doesn’t get to decide what’s taken. Team members should be working with the dentist to understand what the doctor’s prescribing, and from that, they determine the region of interest that they’re taking of the patient. They should also consider what the clinical purpose of the scan is to begin with. Because if we understand our region of interest and the clinical purpose, together those will determine the type of image we should be taking.”
Often, the team will learn that a high dose of radiation is not clinically necessary to scan the requested images, he adds. If, for example, the team needs imaging for pathology, such as an abscess, many dentists may believe that requires a high-resolution scan. But that is not necessarily the case, Garvin explains. “To understand the true clinical purpose, we can often avoid high amounts of radiation,” he says.
How equipment is used is another factor in the amount of radiation a patient is exposed to. Team members knowing how and what to scan can affect overall exposure. To that end, Gochoel says that PreXion emphasizes training for its client clinicians.
“To a certain extent, there is enough variability in taking a scan that it can make a difference, which is one of the reasons why we provide a full day of training,” Gochoel says. “And one of the big aspects of that training is what I would call positioning training. You’re getting the patient positioned properly; removing things, like jewelry, that can create scatter; doing everything you need to do on the front end to grab the best possible image so that additional scans are not necessary—whether that be additional 2D scans or additional 3D scans. The big thing is that the person who’s taking the scan can get that patient positioned and set properly, in accordance with state regulations, so that scan will suffice for treatment purposes for a number of years.”
Doing More With Less
Manufacturers strive to deliver imaging equipment that uses the least amount of radiation possible, and progress has already been made. Currently, all CBCT units offer 2 forms of low-dose radiation, according to Garvin.
CBCT units provide either a low-dose feature on the machine itself or offer what is classified as a low-dose protocol, where the clinical professional designs the exam to limit the use of radiation as much as possible, Garvin explains. “All machines, historically, have had low-dose functions, meaning we lower the amount of radiation to the patient. That’s been around forever. The downside to that is poor image quality.”
To improve the image, manufacturers began to develop what are mostly referred to now as low-dose protocols, Garvin explains. This development lowered radiation and increased scan speeds by going around the patient more quickly, he says.
“Because of the speed, they reduce the number of frames they take during the scan and then use software to clean up the images to make them presentable,” Garvin says. “That’s why they’re called a protocol because it’s not just lowering the dose like all machines have been lowering radiation in the past.”
Although these protocols may seem like a silver bullet solution, no manufacturer has been successful; all these low-dose protocols have failed to maintain the quality of the diagnostic image, Garvin explains.
“The manufacturers are doing what they can, but they still can’t get good-quality images,” he says. “Now, however, Planmeca has created Planmeca Ultra Low Dose™, which was developed in 2014. With our protocol, we do things like other manufacturers, but 1 thing that is different is we still capture the same number of frames during an ultra–low-dose scan that we would during a normal scan. As a result, studies have shown that our machines don’t lose image quality like all the others do. Now we are seeing radiation levels that are equal to or lower than digital intraoral and panoramic images without losing diagnostic image quality.”
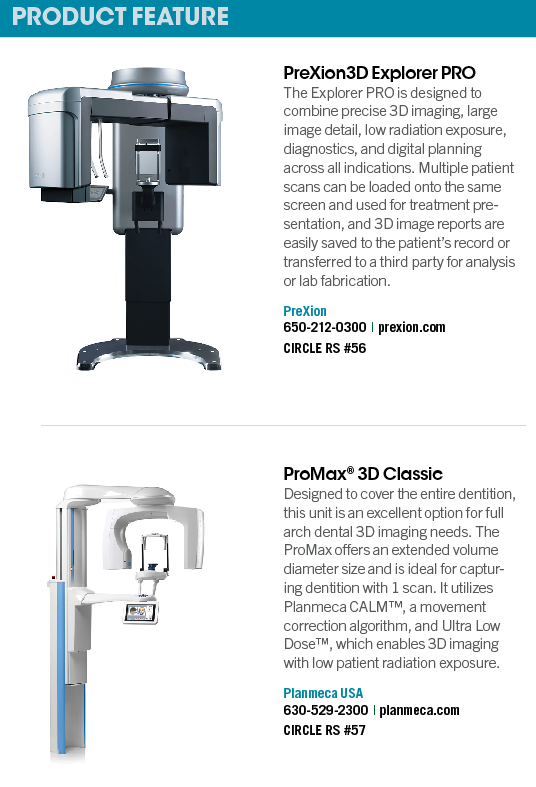
Demand
Diagnostic imaging is a necessary part of the dental practice, and Gochoel observes that larger x-rays are becoming more necessary. “There is a general demand now for larger field of view images than there ever was before,” he says. “There are a couple of reasons for that: No. 1 is that we’re coming out of the pandemic. Doctors are trying to capture more revenue in their practice. Let’s say the average doctor has lost somewhere between 5% and 20% of their patients, because patients are just too concerned with their own health and safety out of fear of catching COVID-19. At this point in time, it’s very common for doctors to be looking for sources of additional revenue, and a lot of patients want airway analysis and sleep apnea treatment. And so that requires a larger field of view to capture the entire airway and look at it. Generally, larger fields of view require more radiation, but one of the interesting things about it, and one of the ways PreXion has gotten around this, is that we’ve developed a larger flat panel detector, which—from a technology perspective—allows the doctor to take that image in 1 complete scan. That’s because 1 scan provides X amount of radiation. Two scans are 2 times the amount of radiation, and then 3 scans would be 3 times the amount.”
PreXion’s imaging technology allows for larger scans with less radiation than other systems. “In order to create that large field of view, others do what’s called ‘offset image’ or ‘horizontal stitching,’” Gochoel says. “In other words, the actual image is a combination of the 2 images. There will either be a vertical stitch that will go straight down through the middle or a horizontal stitch that will go across the image itself. If the patient’s kept very still, there’s not a big issue with it, but the bigger issue comes with radiation exposure in order to get that image, the machine must do 2 passes. Our Excelsior model must take 2 passes to complete a larger [field of view]. The new Explorer model must take only 1 pass to provide a larger and arguably a better image. So, that’s a win-win: a win for the doctor, a win for the patient.”
Computer-Aided Imaging
For as long as imaging has been used in dental, vendors have endeavored to reduce the amount of radiation while delivering high-quality images. “This is an interesting thing from a company perspective,” Gochoel says. “We want to do the best quality, best image clarity with the lowest radiation possible, and so there’s constantly a look at the technology to improve upon that goal.”
Using a computer to essentially fill in the blanks is one way the industry delivers safer images. “Some systems will either use multiple passes or use an algorithm,” Gochoel says. “So, their machine will scan somewhere between 210° to 270°, and then they’ll actually use an algorithm to construct the remainder of the image. It does create scatter and we would prefer to not have to take a second x-ray. We prefer to get it right the first time, because the second x-ray obviously, or the second scan, creates even more radiation. Ours is a full 360° rotation, so there is no image reconstruction used. It captures the image completely around the patient to take the best image possible.”
“Historically, image quality has been developed by humans,” Garvin observes. “So, when it comes to high-resolution 3D scans, the results have typically been noisy and grainy. Today we are utilizing artificial intelligence to resolve the problem with scans for [endodontic] scans, for example. Utilizing machine learning, we can now deliver smooth, clear, high-resolution scans without increasing radiation to the patient. It’s just the beginning of how the new algorithms of the future will be developed.”
OCT
Inroads have been made toward diagnostic images without any ionizing radiation. Optical coherence tomography (OCT) is a technology more often seen in other medical disciplines, but it is starting to get greater adoption in dental.3
“OCT works the same as ultrasound imaging, except that it uses light instead of sound,” says Ruikang K. Wang, PhD, professor of bioengineering and ophthalmology, University of Washington. “It measures the magnitude and echo time delay of back-reflected/backscattered light from internal microstructures in materials or tissues. OCT images are 2D or 3D data sets that represent optical backscattering in a cross-sectional plane or 3D volume. When a beam of light is incident into tissue, it is backscattered differently from structures with varying optical properties, as well as from boundaries between structures. The dimensions of these internal structures can be determined by measuring the ‘echo’ time it takes for light to travel different axial distances.
“Cross-sectional images (or B-scans) are generated by transversely scanning the incident optical beam and performing sequential axial measurements of echo time delay (axial scans or A-scans),” he continues. “This produces a 2D data set that represents the optical backscattering in a cross-sectional plane through the tissue. [Three-dimensional] data sets are generated by acquiring sequential cross-sectional images, scanning the incident optical beam in a raster or other 2D pattern. 3D OCT data contain comprehensive volumetric structural information and can be displayed similar to MRI or CT images.”
Even with no ionized radiation, OCT delivers very fine resolution, close to the level of a single cell size. “OCT can be considered as an optical analog to Ultrasound, CT, or MRI, but with microscopic resolution,” Wang says. “OCT is in a unique position because it enables not only 3-dimensional structural imaging of tissue architecture and pathology but also depth-resolved, 3D imaging of functional tissue information.”4
Though OCT is used in other medical fields, it hasn’t been widely adopted in dental, but Wang expects that to change. “OCT has now become a standard of care in clinical ophthalmology,” Wang says. “However, despite the efforts that have been paid in the research development of dental OCT, its clinical adoption in dentistry is still coming. Because OCT images capture both the hard and soft tissue structures at high resolution, it clearly promises the unique capacity to identify dental disease before destructive changes have progressed, allowing for earlier intervention than is possible with current diagnostic modalities. Together with the need of more rigorous clinical validations by working with dental professionals, further technical innovations in dental OCT device development are needed to make OCT become more prevalent in dentistry—for example, improving its imaging speed, imaging field of view, and, most importantly, the device cost.”
An Abundance of Concern
To some degree, dental faces criticism regarding the amount of radiation to which patients are exposed, but maybe that’s misplaced, Gochoel says.
“If you were sick and you went to the hospital, and the doctor said you needed an x-ray, no one ever bats an eye at that,” Gochoel says, “because that’s what’s recommended for your care. But unfortunately, with that, you’re getting a lot of radiation, whereas on the dental side of things you’re generally not. So, part of it is also from our company’s perspective…while we’re working on the technology, it’s also that we’re trying to educate the consumer through our dentist to give them some points of reference.”
Radiation is seemingly everywhere, and dental x-rays aren’t even the greatest exposure risk. “With one of the standard mode scans on our Explorer PRO CT model, the amount of microsieverts of radiation is equivalent to about as much radiation that you would get on a round-trip flight from New York to [Los Angeles],” Gochoel says.
“So, part of it is also putting it into some perspective. A lot of people don’t realize that just walking around all day, we’re exposed to radiation in different places in our lives. So, that’s a very common one where someone would take a cross-country flight and not think twice about it. And again, it’s much less frequently, because we don’t recommend that doctors take scans continually. We recommend that they be taken about every 3 years.
“The main thing is really around patient’s concern for radiation,” he continues. “Because radiation does have a purpose, and that is, obviously, providing the best image quality possible. So there tends to be a dichotomy around image quality along with radiation.”
Atomic Age monster movies of the 1950s may have bolstered society-wide radiophobia, and, to some degree, that has trickled down to the dental world. To ameliorate some of those concerns, dentists and imaging vendors are doing what they can to limit the amount of radiation to which patients are exposed.
References
1. Ropeik D. Godzilla and the birth of modern environmentalism. Psychology Today. Published June 10, 2014. Accessed May 28, 2021. https://www.psychologytoday.com/us/blog/how-risky-is-it-really/201406/godzilla-and-the-birth-modern-environmentalism
2. Sansare K, Khanna V, Karjodkar F. Early victims of X-rays: a tribute and current perception. Dentomaxillofac Radiol. 2011;40(2):123-125. doi:10.1259/dmfr/73488299
3. Won J, Huang PC, Spillman DR, et al. Handheld optical coherence tomography for clinical assessment of dental plaque and gingiva. J. Biomed Opt. 2020;25(11):116011. doi:10.1117/1.JBO.25.11.116011
4. Le NM, Song S, Zhou H, et al. A noninvasive imaging and measurement using optical coherence tomography angiography for the assessment of gingiva: an in vivo study. J. Biophotonics. 2018;11(12):e201800242. doi:10.1002/jbio.201800242
