Different Uses of Photobiomodulation in Your Practice
PBM can be a game changer in your practice. It is easy to perform and can easily help change your patient’s health.
Those who are Star Trek fans will remember Bones and his tricorder, a device he could wave over a damaged site and repair it almost right before your eyes. Well, photobiomodulation (PBM) may not be as dramatic as the tricorder, but it does use light energy to repair damaged areas for a patient.1 As dentists, we treat the oral cavity, and with the aid of PBM, we can make the patient heal faster and repair a damaged site like a tricorder.2
PBM is used by certain professional sports teams, colleges, Olympic athletes, chiropractors, veterinarians, and dentists. PBM can be used in the dental profession to decrease pain, pretreat for orthodontics, treat erosive lichen planus, paresthesia, angular cheilitis, aphthous ulcers, temporomandibular disorders (TMDs), and prevent infections—just to name a few.3 It is also used in postsurgical applications, endodontics, and periodontics. This article will go over some of the uses of PBM.
PBM is like photosynthesis in plants but is the use of certain wavelengths of light in the red and near-infrared spectrum (ideal range is 660-980 nm). PBM causes intracellular photochemical changes that lead to a cascade of downstream intracellular, extracellular, and physiological changes.4 The mitochondria (within the cell wall) are particularly receptive to this process. At the cellular level, visible red and near-infrared light energy are absorbed by mitochondria, which perform the function of producing cellular energy called adenosine triphosphate.5
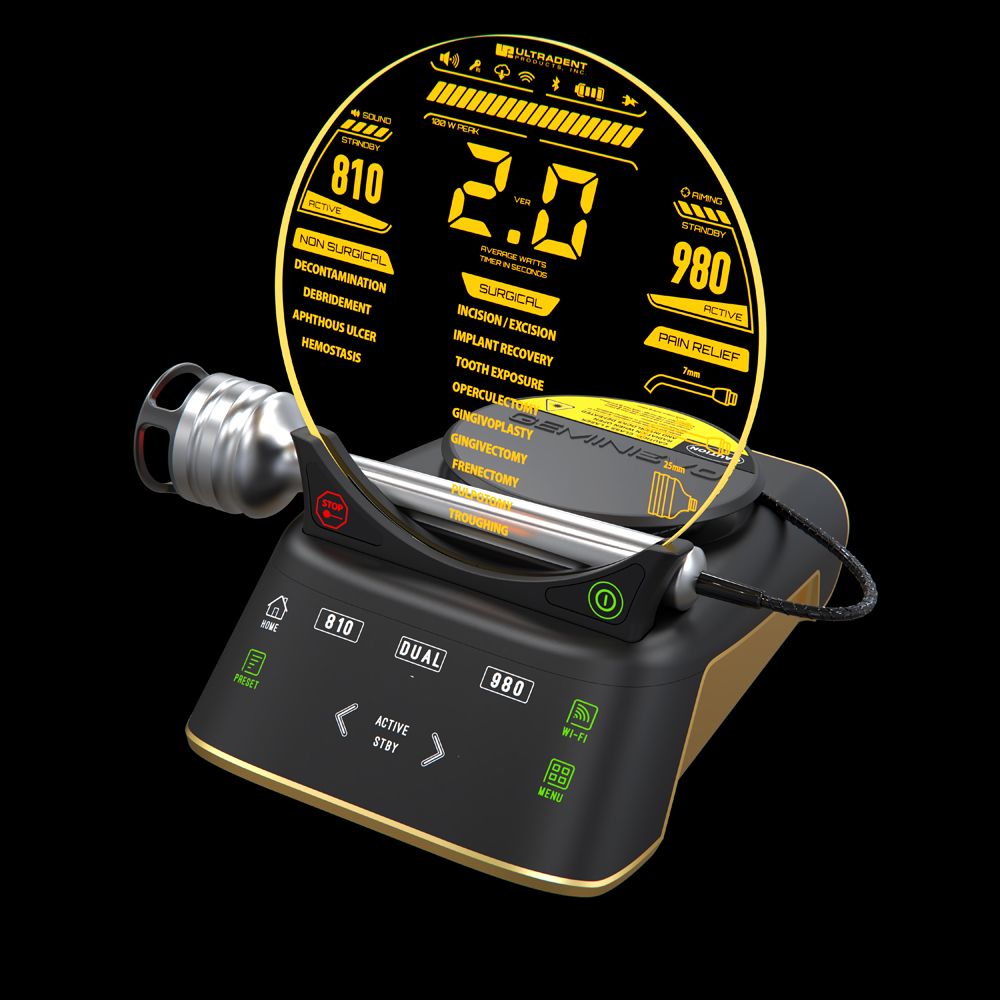
The Gemini EVO laser, used by the author, has 16 preset procedures divided into 3 categories for efficient, intuitive use. Three photobiomodulation (PBM) adapters are included so clinicians can take full advantage of their new dental laser.

The key to this entire process is a mitochondrial enzyme called cytochrome c oxidase, which is a chromophore that accepts photonic energy of specific wavelengths when functioning.1 Cell physiologists have determined that optimal use of PBM is in the range of 4 to 6 J/cm2 of energy, although the therapeutic window appears to be significantly larger than that range.6 This allows the mitochondria to reenergize the cell. Lesser amounts have no effect, and greater amounts have been found to stimulate endorphins.7
Each cell and everyone may react differently to energy, thus it is important to find what works for the patient so you can then continue to treat at that level. One study has shown that every person produces endorphins after surgical procedures—some produce more than others, some produce less than others. The interesting portion of this study is that narcotics inhibit our natural production of endorphins.8
Figures 1 (above) and 2: Approved PBM treatments include treatment for postoperative pain on surgical areas, TMDs, erosive lichen planus treatments for oral mucositis, and others that are associated with pain management.

Endorphins are the body’s natural painkillers, and they are released in the hypothalamus and pituitary gland in the response to pain or stress. Long-distance runners are notorious for pushing their bodies to release endorphins to run faster and go longer distances. The Federal Drug Administration recognizes the use of PBM only for pain management.9 This could include treatment for postoperative pain on surgical areas, TMDs, erosive lichen planus treatments for oral mucositis, and other areas that are associated with pain management (Figures 1 and 2).10
One of the most dramatic cases I’ve treated with PBM to date centered on a patient who presented to my office with a numb tongue. She felt as though it was swollen, and she could not talk correctly. She went to numerous physicians, and none gave her any encouragement to regain feeling back in her tongue. One physician told the patient to carry an EpiPen and to use it if her tongue got extremely swollen. The patient had a biopsy done on the lingual of #29 several months ago. I decided to apply PBM on the dorsum and ventral side of the tongue.
PBM is used by the dental profession to decrease pain, pretreat for orthodontics, treat erosive lichen planus, paresthesia, angular cheilitis, aphthous ulcers, temporomandibular disorders (TMDs), and prevent infections.

After 1 treatment of PBM, the patient could feel a “tension being removed from her tongue.” She had a total of 5 treatments, recovered all feeling back in her tongue, and her speech was normal again.
A second example of a use of PBM is for patients who have a TMD. The patient will likely have pain in a specific site on the masseter. Treatment is to overstimulate the site with over 12 J of energy at the specific site that has the most pain. Next, treat acupuncture points around the ear, then treat the lymph nodes in the head and neck on each side of the face (submandibular and clavicular sites) with 6 J of energy. Treatment for TMD is not a 1-and-done, like most cases of PBM are. These treatments can take over 6 sessions that take place 4 to 5 days from one another.11,12
We’ve only touched the surface of the number of uses for PBM. Some may consider this voodoo dentistry, but it does work, and there are numerous sources in literature and in-person education including the Academy of Laser Dentistry (laserdentistry.org). PBM is a game changer, as it is easy to do and can easily help change your patient’s health.
