A new and innovative approach to treating xerostomia
Why the time is now to initiate conversations with patients suffering from dry mouth.

Xerostomia, or dry mouth, if not effectively managed, can significantly impact oral health and subsequently overall health. For a patient suffering with xerostomia, it’s so much more than simply a “dry mouth.”
Incidence in the US population
Unfortunately we’re not talking about a small segment of our population that’s affected by xerostomia. It’s estimated that as much as 65 percent of the population suffers from xerostomia,1 with the loss of saliva resulting in a devastating cascade of symptoms.
Saliva is essential to the protection, lubrication and preservation of the oral cavity. Like a number of issues we experience in life, the benefit of adequate saliva isn’t fully appreciated until there isn’t enough. Subsequent oral discomfort can range from mild to severe and affect every facet of day-to-day living. The challenges of xerostomia can also present social implications by altering the ability to speak, swallow, chew and digest food. Furthermore, xerostomia has a negative impact on dental caries, plaque accumulation, gingivitis, periodontitis, candidiasis, oral infections, mucositis, burning mouth syndrome and oral lesions.
Etiologic pathways

There are a number of etiologic pathways that initiate a xerostomic condition. One of the most common is medication-induced xerostomia.
“Nearly 70 percent of Americans are on at least one prescription drug, and more than half take two,” say researchers at the Mayo Clinic and Olmsted Medical Center. “Twenty percent of patients are on five or more prescription medications,” according to the findings.2
There are more than 1,100 drugs, both prescription and over-the-counter (OTC), that contribute to or induce xerostomia.1 A number of these xerogenic drugs are the most commonly prescribed medications such as antihypertensives, antidepressants, antihistamines, antiacne, antianxiety, muscle relaxants and opioid analgesics. We see patients every day in our dental practices who are taking some of these commonly prescribed drugs.
Head and neck radiation is also a contributing cause of xerostomia. Gray (Gy) is the unit used to measure the total amount of radiation the patient is exposed to. Typically, head and neck radiation for treatment of oral and oropharyngeal cancer is in the range of 45-70 Gy. In the majority of cases, Intensity-Modulated Radiation Therapy (IMRT) is practiced, delivering a precise dosage of radiation to the tumor with the objective of minimizing collateral damage to the surrounding tissue or salivary glands.
Read more: 3M announces new clinical-grade xerostomia relief spray
A mold of the head and neck area is made prior to the start of radiation therapy, referred to as a radiation mask (Fig. 1). The mask ensures that the head is held in the same position, so the radiation targeting can be exact. Despite best efforts, the end result is severe depletion of saliva - and that which remains becomes thick and ropey.

Fig. 1
Another etiologic pathway is systemic disease, and in particular, autoimmune diseases. Autoimmune disease affects 5 to 8 percent of the U.S. population, 78 percent of whom are women.3 It’s the third most common disease category following cancer and heart disease.4
Sjögren’s syndrome, a chronic inflammatory autoimmune disease, is characterized by dry mouth and dry eyes. The disease is precipitated by lymphocytes leaving the bloodstream and infiltrating into the acinar glands. This migration results in degradation, atrophy and necrosis of the acinar glands, impeding the flow of saliva and tears.
“With upwards of 4,000,000 Americans suffering from Sjögren’s, it is one of the most prevalent autoimmune diseases, with nine out of 10 patients being female,” says the Sjögren’s Syndrome Foundation.5
Sjögren’s syndrome can affect any age group, but most patients are diagnosed in their early 50s. One of the first recognizable symptoms of Sjögren’s syndrome is xerostomia, which often precedes the actual diagnosis of the disease.
Diabetes is yet another disease we see almost daily in private practice. With one in four Americans currently diabetic, it’s forecasted that “prediabetes will climb from 90.6 million in 2015 to 107.7 million in 2030.”
This increased prevalence means that 30 percent of all Americans and 51 percent of all seniors would have prediabetes.6 Not dissimilar to a number of other systemic diseases, one of the first clinical manifestations of diabetes is xerostomia, often present prior to the diagnosis of the disease.
Moreover, diminishing saliva may simply be a sign of physiological aging. The U.S. Census Bureau estimates that by 2020, 54.8 million people will be over 65 years of age, and by 2035 there will be 78 million people - with one in five at retirement age. We clearly have a silver tsunami approaching.7
Continue to page two to read more...
Treatment approaches
The goal of today’s dental professional should include comprehensive assessment of salivary flow, possible identification of causative factors, elevating the comfort level of the patient and the administration of preventive measures to avoid further oral complications. There are a number of conservative lifestyle changes that will assist the xerostomic patient who’s struggling with mild to moderate discomfort. These include reducing the intake of caffeine products, sucking on ice chips, sipping water throughout the day and with meals, avoidance of sticky, salty, spicy or hard foods, limiting alcohol intake, avoiding mouth rinses containing alcohol, chewing xylitol gum, or sucking on xylitol mints (Fig. 2), use of fluoridated or amorphous calcium phosphate toothpastes, using a humidifier at night while sleeping, and the use of lubricants on lips. Of utmost importance is regular preventive dental care and the use of fluoride varnishes proactively or extended contact varnishes on any vulnerable white spot lesions or exposed root surfaces (Fig. 3).

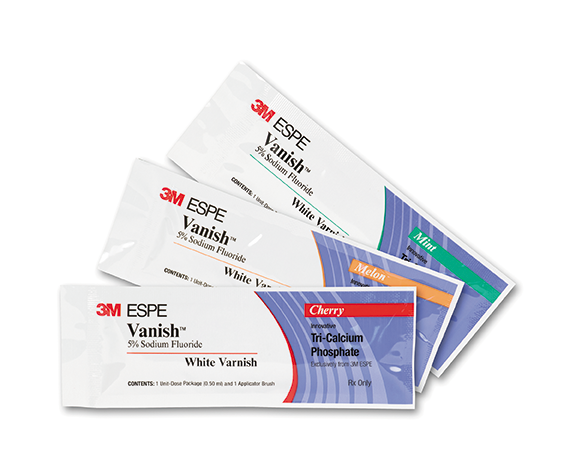
Fig. 2 Fig. 3
An innovative solution
As dental professionals, we want to ensure that our recommendations are not only effective but scientifically supported. A 2011 Cochrane Review began with the following statement, attesting to finding “no strong evidence” that any specific topical therapy (e.g., sprays, lozenges, mouth rinses, gels, oils, chewing gum, or toothpastes) was effective for relieving the symptoms of dry mouth. Although chewing gum was shown to increase saliva production, there was no strong evidence that dry mouth symptoms were improved. The authors noted that “patient preference is an important consideration, together with consideration of the potential adverse effects.”8
The initial results of the Cochrane Review left the dental community with a sense of defeat in being able to recommend a product that would in fact deal with xerostomia effectively. Of further note, and of great importance in the same Cochrane Review, was the statement observing that “oxygenated glycerol triester (OGT) saliva substitute spray shows evidence of effectiveness compared to an electrolyte (or water-based) spray.”
Trending article: The top 5 dental discoveries of 2018
Oxidized glycerol triesters (OGT) have a unique ability due to a lipid formulation to adhere and protect the oral cavity through increased substantivity. There are also studies published in professional journals that scientifically support the OGT technology and its elevated efficacy when compared to water-based solutions. A multicenter controlled parallel-groups trial to evaluate the efficacy, safety and acceptability of OGT spray versus a saliva substitute in the treatment of psychotropic medicines-induced xerostomia resulted in the following: after two weeks of use, patients reported that the OGT spray significantly decreased the initial:
- severity of feelings of dry mouth9
- speech difficulties9
- impaired taste9
The vast majority of subjects attested to the fact that the spray had improved their dry mouth symptoms and their quality of life, and they wished to continue using the spray.
3M Xerostomia Relief Spray (Fig. 4) employs a lipid-based approach to lubricating and moisturizing the oral mucosa with the aforementioned, innovative OGT technology. The lipid-based formulation is insoluble in water, meaning it provides a protective film or barrier that moistens and lubricates with better adherence to the oral mucosa. The prescription-strength spray demonstrates much longer lasting relief, up to four hours, when compared to many other xerostomia prescription medications.

Fig. 4
The streamlined ordering process is accomplished through the online pharmacy, Transition Pharmacy (TPS), which is registered in all 50 states. The prescription is initiated in the dental practice by completing a downloadable form available on the 3M site, followed by TPS contacting the patient for additional insurance and payment information. After the claim is processed, the product is shipped directly to the patient within a few days. TPS will also automatically remind the patient of the next month’s refill requirement.
Making treatment recommendations with the confidence to be assured of efficacy is integral to our day-to-day practice success. It’s also our ethical responsibility to consciously provide our patients with evidence-based recommendations.
Conclusion
As dental professionals, we’re situated on the frontlines of assessing, diagnosing and strategically managing xerostomia both chairside and with self-care recommendations. Are you speaking up for your patients who are suffering from xerostomia by initiating the conversation? A proactive conversation about the symptoms and the impact of xerostomia on both oral and systemic health stands to accomplish a great deal. It may be the initial awareness of a systemic illness that otherwise may have gone undetected or the proactive treatment of an oral condition that would have deteriorated quickly without intervention. We have the solutions to effectively elevate the comfort level of the xerostomic patient, so no one needs to continue to suffer in silence. It’s time to take action!
References
1. The American Academy of Oral Medicine. Integrating Medicine and Dentistry. http://www.aaom.com/index.php%3Foption=com_content&view=article&id=107:xerostomia&catid=22:patient-condition-information&Itemid=120 Accessed November 2018.
2. https://newsnetwork.mayoclinic.org/discussion/nearly-7-in-10-americans-take-prescription-drugs-mayo-clinic-olmsted-medical-center-find/ Accessed November 2018.
3. https://www.sjogrens.org/files/articles/QuickFacts.pdf Accessed November 2018.
4. Fairweather D, Rose, N, Women and Autoimmune Diseases Emerg Infect Dis. 2004 Nov; 10(11): 2005–2011. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3328995/ Accessed November 2018.
5. http://www.sjogrens.org/ Accessed November 2018.
6. Rowley WR, Bezold C, Arikan Y, Byrne E, Krohe S. Diabetes 2030: Insights from yesterday, today and future trends. Popul Health Manag. 2017 Feb 1; 20(1): 6-12.
7. https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html Accessed November 2018.
8. Furness, S., Worthington, H. V., Bryan, G., Birchenough, S., & McMillan, R. Interventions for the management of dry mouth: topical therapies. Cochrane Database of Systematic Reviews 2011, Issue 12.
9. Mouly S, Orler, JB, Tillet Y, Coudert AC, Oberli F, Preshaw P, Bergmann JF. (2007). Efficacy of a new oral lubricant solution in the management of psychotropic drug-induced xerostomia. Journal of Clinical Psychopharmacology, 27(5).
