The top 10 things that scare your patients the most
Is fear keeping patients away from your practice?
Dental anxiety is a serious issue that may be keeping many of your patients away from your office. As many as 15 percent of Americans say they avoid going to the dentist because of fear or anxiety, according to the Cleveland Clinic.

Read more: 6 ways to help patients overcome fear of the dentist
Fear of the dentist covers a range of issues from a fear of pain to fearing the cost of treatment. We talked to dental professionals across the country to find out what scares patients the most - and what you can do about it.
Click through the slides to find out the top 10 things your patients are scared of.


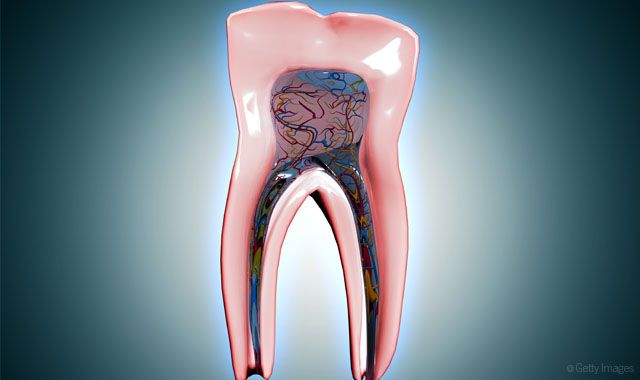
1. Pain
Dr. Jeffrey Lineberry, DDS, has a private practice in Mooresville, NC, where he focuses on complex cosmetic dentistry, restorative dentistry and TMJ/TMD care. After nearly 20 years in practice, he identifies pain before, during or after the treatment as a huge concern for patients. Dr. Lineberry attributes this fear to past experiences where the patient received treatment but wasn’t fully anesthetized.
“That lingers in their mind every time they come in,” Dr. Lineberry says.
Dr. Lineberry uses several methods to comfort patients who are wary of pain during treatment. He gives some patients medications that relieve their anxiety, but he finds that most patients prefer not to use these medications because they don’t like the after effects. Dr. Lineberry also gives patients control of the pace of the treatment, allowing them to use hand signals if they need a break or if something bothers them. In addition to allowing for plenty of time in his schedule for the anesthetic to take effect, he also uses a cold test to prove patients won’t feel a thing.
Related reading: Study finds more than 60 percent of people suffer from dental fear
“I put something very cold on a tooth that was maybe sensitive before, and they don’t feel anything,” Dr. Lineberry explains. “It’s reassuring to know that the tooth is numb before we get started, rather than waiting for the dreaded drill, thinking that the drill is going to hit their tooth and all of a sudden it’s going to hurt.”
However, the best way to combat that fear of pain is building relationships. Dr. Lineberry always reassures his patients that he’s not there to hurt them but to help them. He checks in with patients frequently before, during and after treatment. He says his staff members are also particularly skilled at communicating that they care.
“Reassurance requires a personal touch, patting on the shoulder and their arm. You have to let patients know you are there and that you care,” Dr. Lineberry says.



2. Injections
Kim Miller, RDH, BSDH, says any time dental professionals are doing any procedure where an injection is required, they need to pay particular care and attention to ensure that patients are as comfortable as possible during the injection process. She explains that the pain from an injection isn’t from the needle; the needle is sharp enough that patients don’t feel the needle enter the tissue. Instead, the burning sensation that patients object to results from the cold temperature of the anesthetic entering the warmer body tissue. Miller recommends warming the anesthetic before injecting it to counteract this effect.
“If you don’t have an anesthetic warmer, try using the warmth of your hand to warm up the anesthetic. All anesthetics will be cold right out of the drawer in the dental office,” Miller says.
More from the author: The dental prescriptions that are killing your patients
Using a high-quality topical at the injection site and allowing it time to take effect is another way to ease the discomfort of an injection for patients. Miller, who has practiced for 36 years and coached practices since 1992, says dental professionals should use verbal skills to build value for the procedure that requires an injection to help patients focus on the benefits rather than the drawbacks.
“It’s just like if you go to the doctor and the doctor says, ‘Ok. I am going to give you this shot of B12 in the hip and it’s going to pinch, but here’s why it is such a good idea,’” Miller says. “You can tolerate whatever the discomfort is a lot better if you understand the value that you are receiving in exchange for the discomfort. I can tolerate the discomfort if you tell me what the benefit is.”


3. Triggering sensitivity
Dr. Sarah Jebreil, DDS, AAACD, has a private practice in Newport Beach, CA, that specializes in cosmetic dentistry. She says patients associate whitening with extreme pain from increased sensitivity. Many times, Jebreil says, if they haven’t had it, then they know someone who has.
“That’s a really big fear in our office,” Dr. Jebreil says.
Trending research: Have scientists finally solved tooth decay?
Dr. Jebreil has a few ways she combats this concern for her whitening patients. She has some patients treat their teeth with fluoride in custom trays a week before they come in for the one-hour whitening. If her patients don’t have custom trays or if it was a last-minute decision to whiten, then she uses desensitizing trays by Ultradent. For patients who are super sensitive and too scared, Dr. Jebreil likes to use Kör Whitening. She also encourages patients to take Advil one hour before the appointment.
“If you take Advil and Tylenol two hours apart, you are blocking both the pain pathways,” Dr. Jebreil explains. “After the appointment we have them take Tylenol to make sure they are super comfortable.”
Of course, these measures don’t work for all of her patients.
“One patient we had to give an Ativan to because she was so worried. I think that’s a pretty high fear,” Dr. Jebreil says.



4. Infection
Katrina Sanders, RDH, is an international speaker on infectious diseases, and she says she notices concerns from patients all over the world about infection control. Articles that appear in the global media about dental practices with inadequate sterilization processes spreading hepatitis or HIV to their patient populations influence how patients feel in the chair.
“A lot of times when I open an instrument pack, I have patients ask, ‘Is that clean? Is that sterile?’ They have questions because they have read articles,” Sanders says.
There’s a lot of media coverage about the negative ramifications and risks associated with receiving dental care. However, the dental community exhibits ambivalence about addressing it with patients. Sanders urges dental professionals to acknowledge their patients’ fears and respond to infection control concerns by providing context for the article.
Related reading: The 3 common infections dental professionals should be worried about
“For whatever reason, we turn a blind eye to the more volatile articles that are out there that truly instill a lot of fear in patients. Infection control is definitely a big one.
Hearing about patients who experience major medical emergencies or who pass away in the dental chair, you can’t ignore that. Of course patients are going to worry about whether that will happen to them,” Sanders says.
Sanders says she has a couple of ways she responds to patient concerns. First, Sanders always opens her instrument packs in front of her patients. If her patients do have questions, she walks them through the sterilization rooms at the practice so that they can see the process the equipment goes through during an infection control cycle.
“Every office that I have worked in has an immaculate sterilization area that I am happy to walk the patient though,” she says. “For me, those pieces are very important, reminding them of that.”



5. Cost
The cost of treatment is another significant fear for many patients. Dr. Lineberry says the key to managing this fear is to ensure them that there will be no surprises.
“Let them know up front what their costs will be and what they should expect when they check out that day. Be open and honest about what they need and what it will cost,” he says.
Sanders says the cost of dentistry is relatively manageable. It’s when patients neglect their dental care that things get expensive. However, exercise caution when assuming the fear is about the cost.
Read more: The best ways to help dental-phobic patients
“For patients sitting in the operatory declining treatment, there may be more to it. We tend to think about it like it’s too expensive because it’s easy to use that as an excuse,” Sanders says. “But when we peel back the layers of the onion, there are certainly more pieces to it.”
Dr. Jebreil agrees, adding that she also talks about payment plans and options when presenting treatment options. She confirms any insurance coverage so that patients know what their out-of-pocket expenses will be. However, sometimes she also asks how much it will cost not to have the treatment.
“How much is it going to cost not to be able to smile or chew properly? Reversing it like that and getting the patient to think of it that way helps them see it differently,” she says.



6. Changes in personnel
If a patient usually sees one clinician and then there’s a change in who they see, it can evoke doubt and fear in patients, especially when staff members have different ways of doing things. Miller stresses the importance of the entire team handling appointments the same way, whether it’s a clinical assistant, a dental hygienist or a dentist.
“Continuity and consistency are huge when it comes to helping patients reduce their fear or their anxiety over appointments,” she says.
If patients have to see a different clinician, then Miller advises dental professionals to reassure the patient he or she will receive the same level of care as he or she would with the regular clinician.
More from the author: 10 ways to simplify pediatric dentistry
“I tell my coaching clients to say something like, ‘I know you normally see Sue when you come in for your dental appointments. I want you to know that I have reviewed your chart notes from the last time you saw Sue, and today I am going to take just as great care of you as Sue would take,’” Miller explains.
Miller says another great phrase is “I want you to feel completely safe with me.”
“Patients want to feel safe. When you make a change and you introduce a new team member or a new unfamiliar procedure, it may cause fear. Fear, after all, is about the unknown, so explain all the steps because we want our patients to feel safe with us,” she says.



7. Unfamiliar terminology for treatments
Dr. Jebreil says particular terms can trigger anxiety for the patient. For example, treatments like deep cleaning, scaling and root planing are treatment terminology that can make patients uncomfortable. Some people have anxiety about hygiene already because they had a cleaning in the past that was uncomfortable, so the idea of something “deeper” can be alarming. Dr. Jebreil says to avoid jargon and switch to less threatening words.
“We like to say, ‘comprehensive cleaning.’ It is less scary than deep,” Dr. Jebreil says.
Trending article: Is the solo practice dead?
Another way she treats patients who have anxiety about a new treatment is to do a minor procedure beforehand to prep the tooth so that they’re more comfortable, although it’s really to prep the patient.
“On those patients that are sensitive, we will sometimes pre-polish with PRO-Relief™ by Colgate and that helps calm them down. Doing some sort of procedure before, whether it’s having them wear fluoride trays before they come in for the cleaning or pre-polishing the teeth, is a psychological thing. Polishing or doing the fluoride makes them more comfortable,” Dr. Jebreil says.



8. “New” procedures
People don’t want to be the recipient of something new that the team member has never done before or is trying out, especially in the dental chair. Miller explains that patients want the assurance that whatever it is that the dental professional performs, he or she has the skills and knowledge to handle it. So saying the word “new” before treatment might trigger alarm bells in the patient’s mind.
“I don’t encourage the word ‘new’ at the chair,” Miller says. “I think it’s more appropriate to say, ‘Today, I am going to do something different and here’s why.’”
Related reading: Do your patients trust you?
Any time patient protocols change, whether it’s new radiography equipment or alternative hygiene options, Miller says explaining the change to the patient in a particular way is important. Dental professionals never want the patient to think they’re practicing or unskilled in the technique.
“Let’s say, for example, the hygienist is introducing subgingival air polishing. If I am going to do that for the patient and I have never done it for the patient before, I would not want to introduce it as a new technique. I would want to introduce it as an advanced technique,” Miller explains.
She also recommends telling the patient that the practice has added an improved technology to its armamentarium and he or she gets to experience it today.
“The difference when explaining it like that is the patient doesn’t think that I am practicing something on them,” Miller says.



9. Repeats of past bad experiences
Patients experience a culmination of old fears in dentistry, Sanders says. It starts when they’re young. Previous patient experiences affect the present patient experience often in negative ways - even if it didn’t happen to the patient personally.
“A lot of times our young patients are coming in and are fearful because somebody in the family is fearful and shared terrible experiences about their dental treatment,” Sanders says.
More from the author: 7 tips for designing your dental practice
Another example is when Sanders delivers treatment plans for periodontal disease. Sometimes after she tells them the plan, patients will tell her negative things associated with the treatment such as that it hurt a friend or family member or it didn’t help them much.
Other times people have had medical emergencies in the chair, like fainting, seizures or panic attacks. Many of these patients fear they’re going to have a similar scenario every time they sit in the dental chair. Sanders has had patients tell horrible stories about dentists strapping patients to the chair or putting a foot on a patient’s chest for an extraction. She suggests reminding patients that dentistry has developed better ways to address patient fears.
“I would never want to strap someone to the chair to force them to have dentistry done. There are opportunities for sedation and putting them on various types of medication to reduce anxiety and make it more comfortable,” Sanders says. “Dentistry as an industry has elevated how we address some of our patient fears. It’s important for us to develop more of an awareness of that with our patients.”



10. Fear of the unknown
Dr. Lineberry says many patients experience dental anxiety when they show up for some of their first treatments because of fear of the unknown. Furthermore, patients aren’t looking forward to being judged for the condition of their oral health.
“A lot of patients have been chastised, lectured to or given a hard time about their current dental condition. They are afraid of being talked down to and made to feel ashamed for the condition,” he says.
“A lot of patients come in facing fears of not knowing what their mouth looks like, fear of having cavities or periodontal disease or oral cancer. I think that is a huge fear - the cost of the neglect,” Sanders adds.
Related reading: Are your patients terrified of visiting your practice?
Dr. Lineberry says he sees it as an opportunity to educate the patient. He takes photos with an intraoral camera and then he shows the patient the images on the operatory screens.
“That way they can see what’s going on in the mouth. It helps relieve some of the anxiety. It’s like the old days like we said for kids, ‘tell, show, do,’ Dr. Lineberry says. “Tell them what you are going to do. Show them how you are going to do it. Then, do it.”
Dr. Lineberry also uses a Nikon SLR camera to educate patients. He says it helps with the initial treatment plan process, even more than the images from the intraoral camera.
“They don’t know it as the lower front molar from an upper first pre-molar. When you show them a whole arch picture, you can teach them and say, ‘This is the bottom right. This is the bottom left,’” Dr. Lineberry says. “And then it helps them correspond when they see all their teeth versus just a single tooth or two at a time.”
Miller adds that it scares patients when they don’t know what’s going to happen next in the chair. She sees hygienists begin working on patients, putting their hands in patients’ mouths, without telling them what to expect.
Trending research: Can opioids prescribed for wisdom tooth extraction lead to long-term drug use?
“Not telling them what’s coming and just doing something is not a good idea,” Miller says. “We need to say, ‘Now I am going to do this. Then, I am going to do this,’ and so on to help them understand what the next steps are in that treatment, whatever they might be.”
When it comes to patient fears, Sanders believes the critical message is that dental professionals need to step into the role of altering patients’ perceptions of dentistry.
“It’s no longer dental extractions done by a barber,” she says. “We are highly trained individuals. We have pain management techniques that are effective. We are highly educated in alternative techniques to address our patients’ concerns, whether it be dental hypersensitivity, dental anxiety or dental phobia, and we have plenty of tools in our tool belt. The ability for us to reach patients in a humanistic way can really change the way patients and, in turn, society sees and understands dentistry as an industry.”
