The Role of Extraoral Vacuums During and After a Pandemic
Reducing the potential infectious load of the aerosol in dental practices can be a key weapon in combating COVID-19.

A variety of dental instruments generate aerosols that contain potential pathogens and represent serious health risks to dental professionals. The high-speed turbine handpiece is the most obvious aerosol generator, but instruments such as sonic and ultrasonic scalers, hard tissue lasers, and even air water syringes also contribute to the problem.
To address aerosol-related risks, dentistry has adapted universal precautions for infection control and personal protective equipment (PPE) recommendations. In light of the coronavirus disease 2019 (COVID-19) pandemic, current PPE should include an appropriately rated respirator or mask for the procedure, a face shield, a head cap, a long-sleeved gown, gloves, and shoe coverings to reduce the exposure and potential spread of infectious diseases (Figure 1). These strategies help protect the professional from exposure but do nothing to minimize the potential pathogenicity or control of the origin of the aerosol during the procedures.
Figure 1: A dentist follows new PPE recommendations, a result of the COVID-19 pandemic.

Aerosols have a 60-year-long history in dentistry, and as a result, many professionals have become complacent, casual, and even cavalier in their attitude toward the potential health risks. COVID-19 has presented a long-overdue wake-up call. The health risks go beyond COVID-19 and include a more recently recognized progressive and fatal disease, idiopathic pulmonary fibrosis. In a 2017 report examining 125,000 individuals in 974 types of jobs and their risk of contracting a disease while at work, hygienists, general dentists, dental assistants, and dental lab technicians occupied 4 of the top 5 spots.1
Although notable risks occur from obvious infectious diseases such as influenza, HIV/AIDS, and, more recently, severe acute respiratory syndrome coronavirus and Middle East respiratory syndrome coronavirus, this does not tell the whole story.
Perhaps even more concerning, in 2015, the Centers for Disease Control and Prevention released a report indicating that dental professionals are 23 times more likely to contract and die from idiopathic pulmonary fibrosis.2 Although the mechanism is not completely understood, it is believed that continued exposure to bacterial proteins inhaled from the aerosol contribute to this disease. Dental professionals are dying from this aerosol-borne disease.
Identifying the Risk
The first dental aerosol study was published in 1969.3 In this preliminary study, the investigators defined aerosols as airborne droplets less than 50 µm in diameter. They reported colony-forming units (CFUs) per minute generated from numerous activities, including breathing, talking, coughing, sneezing, and toothbrushing. Talking and breathing produced very few CFUs, whereas sneezing and toothbrushing produce significantly more.
Then, in 2004, Harrel and Molinari described diseases known to be spread by droplets and aerosols, dental procedures that generate them, and best practices to reduce aerosol contamination and exposure.4 In their study, they identified the high-speed drill, ultrasonic units, air polishing, the air-water syringe, air abrasion, and hard tissue lasers as potential aerosol-generating devices. They recommended best practices to reduce the aerosol risk, including recommended PPE, high-volume evacuation, preprocedural rinses, and high-efficiency particulate air (HEPA) room filters.
Multiple studies recognize the aerosol risks from the ultrasonic handpiece and the importance of controlling the aerosol.5,6 There are conflicting data on whether routine use of rubber dams increases or decreases the aerosol risk.7 Additionally, there is a lack of data to demonstrate that N-95 respirators are better than level 3 surgical masks at preventing disease transmission to the dental professional.8
Reducing Exposure
Extraoral HEPA vacuums can reduce the aerosol exposure to dental professionals (Figure 2). A HEPA filter removes 99.97% of particulates 0.3 µm in size and larger. Numerous studies looking at bacteria have documented the efficacy of HEPA filters to remove pathogens.9-11 However, although HEPA filters efficiently remove bacteria-size particles, which are captured by filtration, they are not efficient at removing virus-size particles, which are generally less than 0.3 µm; the COVID-19 virus is about 0.12 µm. An obvious problem then arises during a viral pandemic, when significant percentages of people who are actively spreading the virus have no symptoms.
Figure 2: A dental procedure is performed with an accessory extraoral vacuum.

A virus attached to a water droplet or other particle 0.3 µm or larger will be captured in the HEPA filter by a process termed inertial interception and impaction because the particle is larger than the pore size of the filter and gets trapped or filtered out of the airstream. Thus, this type of filtration is dependent on the pore size of the filter.
HEPA filters can also be very efficient at trapping and removing particles from 0.3 µm down to 0.003 µm, at 99.995%, but this is dependent on the air velocity moving over the filter. These extremely small particles, including those the size of the COVID-19 virus, can be removed by a process called diffusion physics (Figure 3).12 Diffusion occurs by a combination of Brownian motion and van der Waals forces.13
Figure 3: Graph of HEPA Filtration Physics, NASA. KEY: HEPA, high-efficiency particulate air.
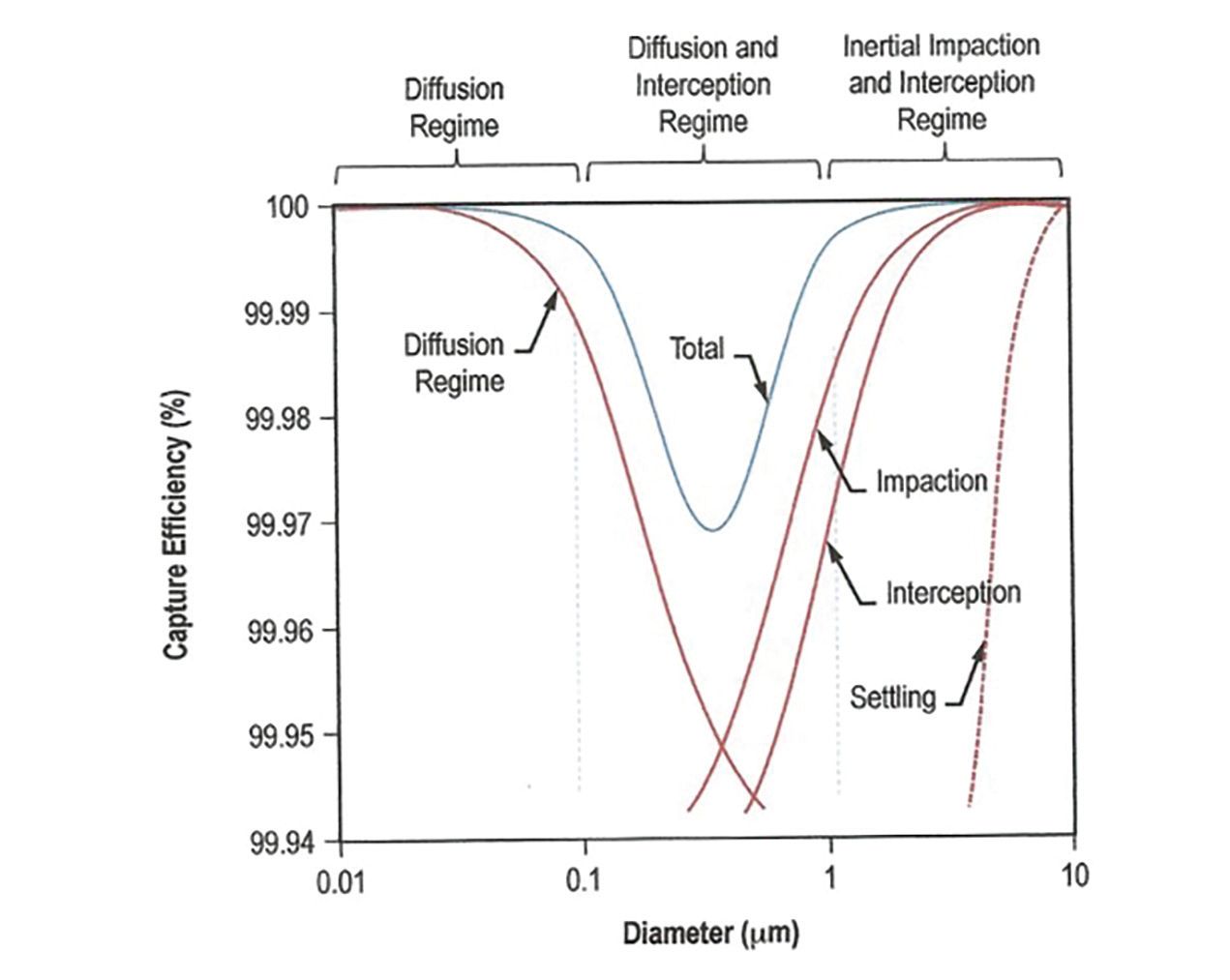
Suffice it to say that removal of particles larger than 0.3 µm is filter pore size dependent, whereas removing smaller particles is strictly a function of air velocity. This velocity requirement has been studied and established by NASA research to be 2.5 to 5 linear feet per minute, or less than 0.06 mph.12
So, the current challenge in virus transmission in the dental aerosol involves the ability to move the air fast enough to capture all the aerosol at the source, the patient’s mouth, and then bring it down to extreme slow velocities over the HEPA filter interface to actually capture the virus-size particles—but it can be done (Figure 4).
Figure 4: Dental Safety First’s DAX, an extraoral HEPA vacuum, is designed to remove virus particles.

Heeding the Wake-up Call
The science is clear: Dental aerosols pose serious health risks for dental professionals. The COVID-19 pandemic issued a long overdue wake-up call for the dental profession to recognize the generalized health hazards of working daily in these aerosols.
It’s time to take control of the aerosols and reduce these risks for ourselves, our teams, and our patients. Extraoral HEPA-filtration vacuums can be designed and calibrated to remove not only bacterial particles but also virus-size pathogens. When used routinely for all aerosol-generating procedures, pretreatment rinses and extraoral vacuums offer new solutions to reduce the transmission of deadly diseases during dental treatment. ●
References
1. Kiersz A, Gillett R, Hoff M. 47 jobs that will always be bad for your health, and how much they pay. Business Insider. July 14, 2020. Accessed July 24, 2020. https://www.businessinsider.com/most-unhealthy-jobs-in-america-2017-4
2. Nett RJ, Cummings KJ, Cannon B, Cox-Ganser J, Nathan SD. Dental personnel treated for idiopathic pulmonary fibrosis at a tertiary care center - Virginia, 2000-2015. MMWR Morb Mortal Wkly Rep. 2018;67(9):270-273. doi:10.15585/mmwr.mm6709a2
3. Micik RE, Miller RL, Mazzarella MA, Ryge G. Studies on dental aerobiology. I. bacterial aerosols generated during dental procedures. J Dent Res. 1969;48(1):49-56. doi:10.1177/00220345690480012401
4. Harrel SK, Molinari J. Aerosols and splatter in dentistry: a brief review of the literature and infection control implications. J Am Dent Assoc. 2004;135(4):429-437. doi:10.14219/jada.archive.2004.0207
5. Singh A, Shiva Manjunath RG, Singla D, Bhattacharya HS, Sarkar A, Chandra N. Aerosol, a health hazard during ultrasonic scaling: a clinico-microbiological study. Indian J Dent Res. 2016; 27(2):160-162. doi:10.4103/0970-9290.183131
6. Su J. Aerosol transmission risk and comprehensive prevention and control strategy in dental treatments. Article in Chinese. Zhonghua Kou Qiang Yi Xue Za Zhi. 2020;55(4):229-234. doi:10.3760/cma.j.cn112144-20200303-00112
7. Al-Amad SH, Awad MA, Edher FM, Shahramian K, Omran TA. The effect of rubber dam on atmospheric bacterial aerosols during restorative dentistry. J Infect Public Health. 2017;10(2):195-200. doi:10.1016/j.jiph.2016.04.014
8. Smith JD, MacDougall CC, Garber GE. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. CMAJ. 2016;188(8):567-574. doi:10.1503/cmaj.150835
9. Noro A, Suyama Y, Takahashi E, et al. The effectiveness of the “Clean-Area-System” for infection control in the dental clinic. Bull Tokyo Dent Coll. 1998;39(1):15-24.
10. Teanpaisan R, Taeporamaysamai M, Rattanachone P, Poldoung N, Srisintorn S. The usefulness of the modified extra-oral vacuum aspirator (EOVA) from household vacuum cleaner in reducing bacteria in dental aerosols. Int Dent J. 2001;51(6):413-416. doi:10.1002/j.1875-595x.2001.tb00853.x
11. Jacks ME. A laboratory comparison of evacuation devices on aerosol reduction. J Dent Hyg. 2002;76(3):202-206.
12. Perry JL, Agui JH, Vijayakumar R. submicron and nanoparticulate matter removal by HEPA-rated media filters and packed beds of granular materials. NTRS-NASA Technical Reports Server. May 1, 2016. Accessed July 24, 2020. https://ntrs.nasa.gov/citations/20170005166
13. Radiation Protection Systems. Engineering Data for Selecting and Using Portable HEPA Filtration Units and Accessories for Nuclear Applications. Radiation Protection Systems; May 2011. Accessed July 24, 2020. https://imageserv10.team-logic.com/mediaLibrary/261/Engineering_Handbook_rev_5-13-11_-_sm.pdf
