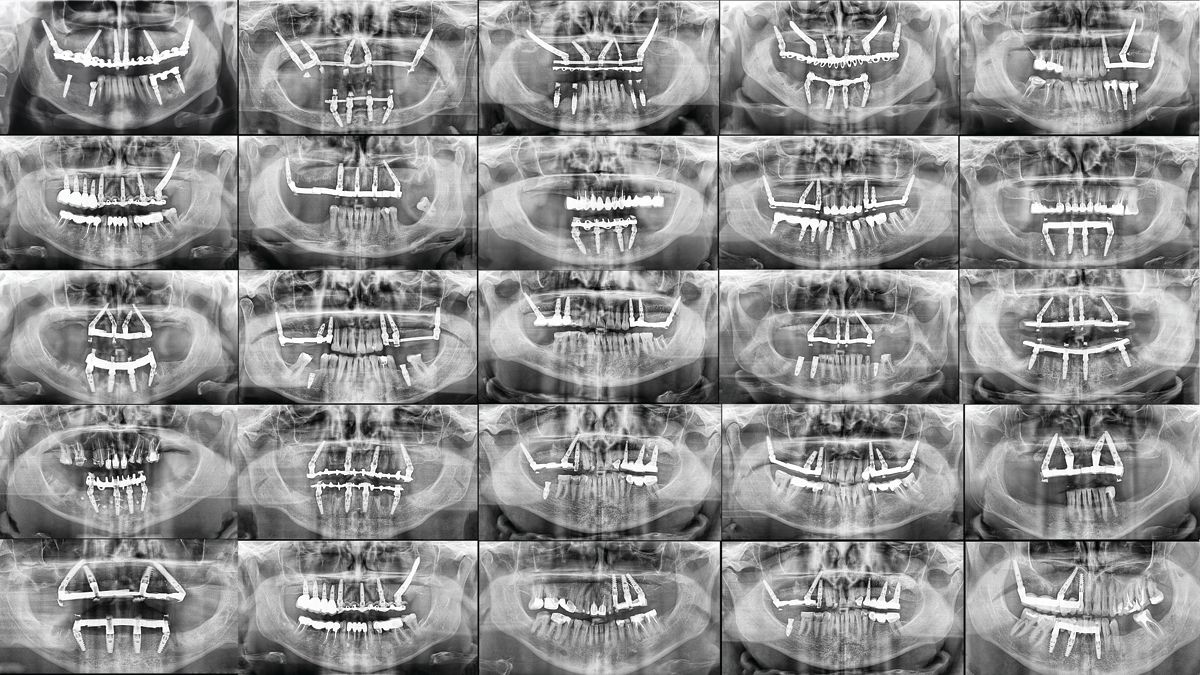
Ghost of Implants Past
Learning from poor past implant placements can help improve future outcomes.
Ghost of Implants Past. Image credit: © Dental Pro Content - stock.adobe.com
In Charles Dickens’ immortal classic, A Christmas Carol, Ebeneezer Scrooge is visited by 3 ghosts: the ghosts of Christmas Past, Christmas Present, and Christmas Yet to Come (technically, he’s visited by 4 ghosts, but Jacob Marley is irrelevant to this discussion).
Dental implantation—and the resulting patient care—can mirror the classic story: Learning lessons from the past can help improve future patient outcomes.
Problems
One of the most common implant problems, observes Catapult Education founder Lou Graham, DDS, is peri-mucositis.
“Peri-mucositis is inflammation in the tissue—without bone loss—around an implant,” he says. “The first identifiable problem would be bleeding on probing, bleeding on brushing around an implant. So if you know it’s a common problem, how do you avoid it? One solution to solve this issue is to place an implant with at least a minimum of 2 mm of keratinized tissue. So if a patient comes back to you and they have bleeding on probing and they do not have attached tissue, one of the immediate solutions is to have a tissue graft placed such that we can minimize the cause of lack of keratinized tissue.”
All too often, peri-mucositis can lead to peri-implantitis.
“Plaque accumulation happens faster around an implant,” Dr Graham continues. “And because it can happen faster, without proper keratinized tissue, further problems such as those described occur down the line. So in essence, they should be thinking about this before. Peri-mucositis can occur immediately, whereas peri-implantitis often becomes evident later on.”
As one might suspect, implants can be affected by other issues in the oral cavity.
“The literature for decades has shown that if other areas of the mouth have periodontal disease, then those bacteria can contribute to periodontal issues involving implants, again bringing us back to peri-mucositis as a precursor to peri-implantitis,” Dr Graham says. “Imagine you have an implant placed in the No. 19 area and you have periodontal disease in other quadrants of the mouth. That implant has a much higher chance of periodontal issues. So I think what dentists routinely do is only focus on the implant and not the overall condition of the mouth. My recommendation: Focus on the entire dentition.”
The Past
The first ghost took Scrooge back to his youth, a time when he had optimistic aspirations. That is also the case for implants. Patients and dentists have a vision for how dental implants can improve a patient’s life. Regrettably, sometimes that vision does not come into focus, especially as complications arise.
On the clinicians’ end, there are several factors that can come back to haunt a case.
“There are many, many factors that determine ‘successful’ implant placement,” Sam Shamardi, DMD, observes. Dr Shamardi is an American Board of Periodontology and Implant Surgery diplomate, faculty member at Harvard’s School of Dental Medicine Division of Periodontology, a member of Catapult Education’s speakers bureau, and the author of The Financial Survival Guide for Dentists.
“It would be incorrect to assume 1 or 2 primary factors are all that it takes, as each case and patient situation is truly unique,” he notes. “That being said, some of the main factors for improper placement include poor initial planning, poor angulation, insufficient bone height/width, incorrect implant size/length choice, excessive heating of drills and/or using dull drills, improper site preparation, not taking radiographs during placement to confirm proper positioning and angulation, poor visibility due to poor flap management.”
The implant itself isn’t the only component that can lead to a less-than-ideal restoration. The appliance attached to it is also a factor.
“We’re talking so much about the implant itself, but there’s also the restorative component,” says Richard Lipscomb, DDS, a general dentist in Mitchellville, Maryland, and a member of Catapult’s speakers bureau. “How does the crown look or how does the bridge look? Is it in the right position? Does it look like it’s in the right position and is it functioning for the patient? Both of those things are important when it comes to an implant, as opposed to a regular crown and bridge. Because of the money and the time involved, patients’ expectations of it being a certain way are higher than anything else.”
The implant’s location can have an impact on whether the placement is negatively perceived.
“In the posterior,” Dr Lipscomb says, “the look of the restoration does not have to be perfect. In this area, we’re dealing with a larger missing tooth or missing teeth, and it’s more about function. In the anterior, it needs to be more Hollywood, because that’s what patients’ expectations are. When you’re dealing with teeth in the esthetic zone, you’re also dealing with implant placement with specific angulation requirements.”
Happily, we don’t have to wait for the future for things to improve for clinicians.
“Technology and software have come a long way, to the point of having the option for guided surgery and surgical stents that can significantly direct clinicians to place more accurately and with fewer risks,” Dr Shamardi says. “However, even then there is a chance for error—or even for poor guide fabrication—which doesn’t match up with the clinical situation. Thus, the dentist has far more chances of doing things ‘better’ now than before, but you still need a good grasp of fundamentals regardless of what experience level and technology.”
Nascent technologies and treatments improve over time and dental implants are no different.
“The hardware has gotten better and implant surfaces are far more streamlined now,” Dr Shamardi says. “However, knockoffs still exist that can be problematic. Original blade implants were a disaster and not predictable; on the flip side, the sheer number of implants placed today combined with the higher number of inexperienced clinicians placing them has created a situation where complications have also risen significantly and some studies quote 20% to 25% peri-implantitis after 2 years so despite better technology, we are struggling with more complications. Stricter standards on who can place implants would help; dentistry is an open border and there are no real guidelines or enforced rules to prevent clinicians with no surgical experience from placing however many they want.”
Dr Lipscomb observes that implants, historically, tend to be largely successful, but most problems tend to stem from overloading implants—too much load or too soon of a load.
“Implants have a high success rate,” Dr Lipscomb says. “And it’s up to the restorative doctor to manage the load placed on implants. Are we waiting 3, 4, or 6 months, a year? Are we putting on a single crown? Are we loading it up with a full-arch, fixed restoration? All those things play a part in terms of, did this implant fail because of poor placement or just overloading it? In most implant cases that fail, it’s the overloading and not so much poor placement.”
Implant restorations are improving, Dr Graham observes, because the 3 components comprising a restoration are in better harmony with each other.
“The machining of implants has gotten better, meaning the fit of the abutment, the crown and the abutment, the abutment to the implant. The machining has gotten better over decades,” he says. “There’s no question about it. So that fit is important because it minimizes bacteria. They continue to come up with different surfaces for faster integration.”
The Present
One of the best advances for dental implantation is improved imaging. Thanks to 3D imaging technology, there’s less guesswork in placement planning.
“Imaging is a big boost,” Dr Shamardi says. “Having 3D technology changes the planning and execution phase and has given rise to guided surgery and stent fabrication. Standard-of-care arguments are trickier, however. Cone beams are an expensive investment that not every office is able to invest in, and many patients still fear radiation even though CBCT [cone beam computed tomography] tech is very safe and shouldn’t be a major concern. Also, there are cases that are ‘easier’ and may not require all the extra bells and whistles, so saying it has to be used for every single case is a tougher case to make. Nevertheless, the information gathered from CT scans is invaluable and makes a noticeable improvement in overall outcomes.”
“Twenty-five years ago, we were using Panorex and radio-opaque markers to estimate bone levels and where to place an implant,” Dr Graham says. “Today, with CBCT technology, we can create ideal surgical stents for proper placement with the idea that placement is restoratively driven. In our practice, our implants are placed accordingly with surgical guides. We then know the restorative end point has already been treatment-planned into the placement, vs years ago when they were just placing implants in bone and then the dentist would have to restore it. As a result, we have far better angulation, far better placements today than we did 25 years ago. I know, many doctors feel that there are many times that guides may not be necessary, but as a restorative dentist, I can absolutely say, ideal placement is not easy without a guide.”
How Patients Live With Poorly Placed Implants
“One of the most common problems that can occur in as little as a few months is open contacts,” Dr Graham says. “Per Tarnow’s studies and others, open contacts can develop in up to 60% of implant casework. We have all seen them become bigger problems for our patients. We all have heard our patients comment about food impaction around an implant, and this often leads to gingival inflammation and/or adjacent tooth decay on the neighboring teeth. One of the solutions is to fabricate patients a retainer when you deliver your implant to minimize tooth movement. Another solution during hygiene visits is to utilize a product called Hybenx around inflamed tissue, around implants and natural teeth. We reviewed this product with our Catapult evaluators and this is a must-have in all of our practices as part of our treatment.”
Sometimes problems can be mitigated by replacing or adjusting the crown or bridge attached to the implant.
“Materials have gotten better over the years,” Dr Lipscomb says. “So now we can use a different material that could be stronger, better, and compensate for the issue with the lack of contact and trying to solve that problem.”
But in the grand scheme of things, it isn’t just the replacement where problems can arise. Patients must do their part, and it’s a good reminder for them to keep up on their at-home care.
“Patients live with horrific periodontal disease and decay far more and far longer than they do with poorly placed implants,” Dr Shamardi observes. “Management wise, there are considerably more options today than before. Too much attention is placed on the procedure itself and not on the management, which is really what makes or breaks the case over the long run. Once an infection establishes itself, it becomes a salmon-swimming-upstream situation and treatment and predictability are far less than they are with maintaining natural teeth, to the point some literature has mentioned reconsidering removing so many teeth in place of implants. That being said, we have numerous options from in-office air polishers and various biofilm-attacking gels and powders to at-home custom peroxide trays via Perio Protect, water flossers, implant-specific flosses, and mechanical brush heads. Thus, we have far more options and the key to success is managing the biofilm and doing whatever possible to prevent and/or minimize complications.”
The Future
Scrooge knew if he didn’t change his ways, bad things would happen. Happily, dentists tend to be more proactive than Ebenezer Scrooge was. Implant dentists are always on the lookout for ways to improve their care.
“The biggest difference with the implants that I do, which are small-diameter implants as opposed to traditional implants, is the size,” Dr Lipscomb says. “And when a small-diameter implant fails, we remove the implant, let everything kind of heal back in the soft tissue, in the bone. And then now we’re back to square one. Because they’re small, the space isn’t very big in the bone. It’s basically like taking out a tooth where with most teeth—medium size to small—we can just take out the teeth, then everything heals up and then we go from there in terms of what are we going to place. We’re going to place a regular bridge or we’re going to place an implant.
“But when you’re dealing with the traditional implant, which is bigger, it’s not a simple thing,” he continues. “I’ve got to take out the implant, then I’m going to have to do a bone graft to replace that space. So it’s never going to be a situation where I’m taking out an implant and then I’m just going to let it heal. It’s more involved because of the types of bone-grafting materials that we have now. I don’t feel that the specialists or surgeons or the periodontists shy away from that area because of a failing implant, meaning they’ll take the implant out, clean out that area, do a bone graft, and now we’re back to a new slate that can be ready for another implant. They’re of that mind-set. Now with that, the issue comes down to, OK, now that we have this new slate, what are we going to do?
“Are we going to change the angulation and are we going to change the type of restoration that’s going to go on top of this implant?” he continues. “Because we know that this was done in the past and it failed. So that’s something different moving forward. And that is going to either be a combination of changing the angulation, changing maybe the size of the implant, and then also changing the restorative options that were used so that it’s not going to be the same as the failed situation.”
If an implant case must be replaced, like so many other dental treatments, a number of factors go into its rectification, but the sooner treatment occurs, the better.
“Implant replacement rate of difficulty varies, again, case by case and depends on the situation, and the reason for the failure itself, along with how soon the problem is identified and treated,” Dr Shamardi says. “Earlier-stage intervention vs later makes a difference, and the source of failure [bacterial vs mechanical/occlusion vs implant fracture] also make a difference in terms of how the removal process will go. Implants that are heavily infected and mobile are easy to remove; those that still have anchorage may require further bone removal. All cases do require regrafting and reestablishment of bone support and some cases will require soft tissue as well; however, once fully treated and with proper healing time the sites can be reentered for a new implant. But there still have to be other considerations such as esthetics, for example, to take into consideration or possibly requiring sinus work. Thus, replacement can become a bigger ordeal depending on the case and, again, varies among many factors.”
”Success” Can Mean a Lot of Things
“I would tell you that defining success of an implant is a variable,” Dr Graham says. “What is success of an implant? Is the success of an implant zero bone loss? Zero bleeding on probing? Total tissue health and no bone loss? And I would say that’s a successful implant. And then you get into, at what point is an implant a total failure? And a total failure, without question, is when an implant is loose. That is absolute, total failure and it must be removed. And the gray zone is how much bone loss has occurred before an implant really needs to be removed and replaced.”
Ultimately, Dr Graham observes that success comes down to 3 things.
“There must be enough bone, along with ideal connective tissue, and finally proper function,” he says. “All 3 must work for long-term success. In regard to a failing implant, one has to evaluate all 3 of the above factors and determine if the implant is salvageable or not. I feel one has to work closely with their specialist in such discussions [unless the general practitioner is trained in all phases of treating this themselves]. If removal is required, routinely, you’re dealing with an ongoing infection, and with such you’re not going to immediately place an implant back into an infected area. Once again, this may involve a potential temporary restorative solution and this is why you must work closely with your surgeon [unless you are performing both the surgical and restorative procedures].
“Ideally, implants would be optimally placed to begin with,” he continues. “But it doesn’t end there. Both patients and clinicians must maintain the implants for the long term. This is a team effort, both via the hygienist and the patient’s home care protocols. Again, knowing that implants have inherent risks necessitates great communication and planning with the entire dental team. Let’s take a common situation where a patient has areas of localized ongoing issues of bleeding on probing and has gone through periodontal hygiene procedures and potentially surgical and nonsurgical approaches, and yet they still have isolated areas of bleeding on probing and probings beyond 3 mm. We all have these patients in our practice, and the question is How best do we prevent further periodontal issues and, equally important, preserve the tissues around the implant/implants? One solution I have used for 8 years is a system called Perio Protect, and this is a system/product that both dentists and hygienists should be educated on. Perio Protect is a system based on [a Food and Drug Administration]–approved custom, lab-fabricated tray with a gasket-type seal. This seal is the key as it keeps a hydrogen peroxide gel in direct contact with the gingival pockets. By wearing these trays 10 to 15 minutes a day, you have a true oxygenation occurring within the pocket and those anaerobic biofilms are placed now in a far more defensive mode. Add sonic brushing and sonic flossing [Slate will redefine flossing] and you have now a far more preventive approach for your implant patients. One additional hygiene product to consider would be the water flosser, but we only recommend the plaque seeker tip. If you aren’t aware of this tip, Google it…it’s the only tip we recommend with the water flosser.”
Scrooge was haunted by the ghosts that visited him that Christmas Eve, each teaching a valuable lesson, leading to his ultimate redemption. Dentists heeding the lessons learned from poorly placed implants can help patients avoid their own nightmares.
