Getting a Clear View of 3D Imaging
The technology, benefits and usage are all on the rise. Find out how 3D imaging can help your practice and your patients and whether this is a great fit for your practice.

You've done it so often that it can be successfully accomplished blindfolded, on a roller coaster or during a hurricane: The patient needs a crown so you get out the polyvinyl siloxane, make an impression and, when the lab has finished its work, you get the new restoration, prepped and ready for placement. That’s how it’s been done forever. Two-dimensional periapical scan data is useful, but, in the 21st century, there’s a way to get that job done faster, more efficiently and with superior results.
Not only do 3D scans eliminate the need for taking physical impressions, but once a scan is acquired, it can be delivered electronically to your lab, resulting in faster cases, start to finish. Even speedier still, if you have a chairside setup, you can produce crowns the same day.
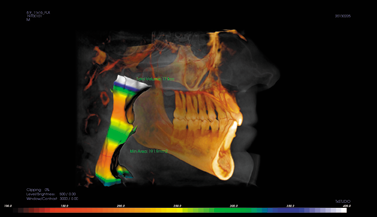
For even more advanced procedures, like implants, cone beam computed tomography (CBCT) allows you to see the patient’s bone structure, allowing better placement of implants and helping discover hidden issues before they become unwelcome surprises during a procedure.
Trending article: The top products of January 2016
History
According to Dr. Dale Miles, DDS, an oral maxillofacial radiologist in Fountain Hills, Ariz., 3D imaging was introduced to North America in 2001, but it took several institutions like the Loma Linda University School of Dentistry and the orthodontic community for it to truly find regular use.
“Dentists looked at CBCT, initially, because of the quality of the scan, the low dose and the fact that they can get some 3D information out of it,” Dr. Miles said. “It was here as early as 2001, but adoption in earnest really began probably in 2005 or 2006 when some more robust machines that were smaller and lighter and easier to put in offices came along.”
Over the past couple of years, popularity and prevalence of the machines has picked up.
“There are people who actually sell their original machines to either upgrade to different-sized volume or a different machine because they were not happy with either service or image quality,” Dr. Miles said. “There’s been an explosion, especially when you throw in the capability of using similar digital data to capture scan data with models without impression materials, which was always a pain. From 2011 to now, it’s accelerated. It really is growing much faster than actual intraoral digital imaging is so it’s here to stay. It’s only going to get better. This is a tremendous imaging modality, but that’s all it is, by the way. It’s just another tool to capture image information.
Trending article: The mental state of today's dentist
Different flavors of digital imaging
Three-dimensional imaging affords doctors and labs never-before-available views of patients’ anatomy.
“You’ve got multiplanar views. We’ve never had that in dentistry,” Dr. Miles said. “By that, I mean we have gray scale images in thin slices and very high resolution-thinner than even medicine. Our slice thickness for these 2D images is less than 0.1 millimeter in some cases, whereas in medicine, one millimeter is their smallest. And in those slices, like medicine, we can get three planes of section. So if you’ve got multiple thin-slice data to find small disease changes, like we do in dentistry, i.e. cavities, bone loss and periapical lesions, that’s a huge advantage. Endodontics is the prime example. Finding canals is easier. Seeing the structure of the canal is easier.
Trending article: The Chicago Midwinter Meeting: What to see in the Windy City
“And then you get to 3D,” he continued. “The 3D allows us to have full-surface reconstruction to show us exactly what the patient’s mandible looks like or maxilla or what the air spaces look like inside of the head. It really is a remarkable technology, and it’s very low dose. It’s not going to replace conventional CT, but it’s a stunning addition as a complementary technique.”
While 3D scans are great tools for doctors, they are also useful for everyone involved in the case. Their digital nature allows for easy communication between everyone in the workflow.
“It allows an even playing field for surgeons and general dentists when placing implants,” said Jason Rogers, restorative sales manager at Henry Schein. “It makes a lot of surgical procedures more accessible outside the specialist network whether it’s oral surgeons or periodontists. Therefore, you have a lot more patients who will have the benefit of working with 3D imaging whether it’s with the grafting procedures or surgical procedures.”
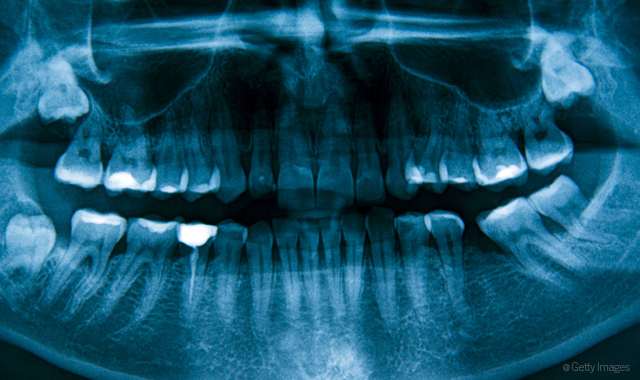
What doctors can do with digital imaging seems to depend on what they want to use it for. Panoramics and periapicals still have their place, but, as more and more doctors bring 3D into their practices, they find increasing uses for them.
Trending article: The top overlooked technologies your dental practice should be thinking about
“There are some offices out there that, I think, their basic policy is if they have a 3D device, almost everybody that walks in the door as a new patient gets a 3D scan,” said Dr. John Flucke, chief dental editor and technology editor for Dental Products Report. “I’m not at that point yet because most of the 3D devices on the market still provide more radiation than just a standard panoramic,so what I prefer to do for the majority of new patients is take a digital pan, bite wings and then PA images as needed, and those are all 2D. But then the 3D stuff is for dental implants. We do TMJ, root canal retreatments and also some fairly complicated restorative treatments, and all of those situations, as well as kind of weird diagnostics stuff that we just can’t figure out what’s going on for whatever reason, those, in my office, are the big things for 3D.”
Cone beam scans are the latest version of scanning technology and offer even finer, more accurate and robust details. They also use less radiation than other scanning modalities and are safer for the patient.
In many cases, different types of scans are used in conjunction for different aspects of a restorative case.
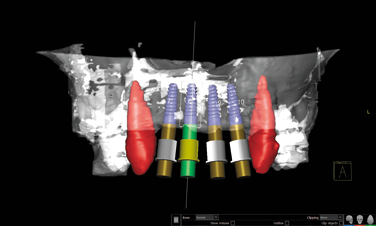
“With cone beam, we’re looking at bone structure so cone beam is going to be used more with implant planning and things like that whereas with surface scans we’re going to be doing crown and bridge,” said Mark Ferguson, assistant manager at Core3dcentres in Las Vegas. “For implant planning, we’re going to need both that surface scan as well as the cone beam, and we’re going to need to line them up together so we have all the data of what’s going on in the patient’s mouth, including where the bone is and where the teeth are. And then we can start to plan, basically, from the tooth down into where the implant should be and what angle is going to be optimal for everything.”
Related reading: Why one Arizona dentist calls 3D imaging a "game-changer" for his dental practice
Tais Clausen, CTO and cofounder of 3Shape, maker of the TRIOS digital impression system, observes that CBCT data delivers the information doctors and labs need for the best patient outcomes.
“With the types of procedures being performed today, especially within the fields of implantology and orthodontics, it’s imperative that doctors and technicians take advantage of 3D CBCT data,” Clausen said. “The ability to see bone, teeth roots, nerves and more makes the planning and diagnostics so much simpler and safer and the patient outcome, more predictable. Doctors and labs want to be able to work with consistent data sets. They need to know they can maintain the tooth setup and vertical orientation established for a patient throughout each part of their planning and restorative aspect. That’s why integrations between our Dental System and Implant Studio software, for example, are so important. The data gets seamlessly shared between lab and practice and remains consistent throughout to give professionals a full and predictable picture of the patient anatomy and create what we like to call the ‘digital patient.’ That insight is just not possible without CBCT scanning.”
3Shape offers practices a variety of TRIOS digital color impression solutions, and the company will soon release the X1, a fully integrated CBCT scanner.
To help doctors get the most out of cone beam data, Dr. Miles sells software called EasyRiter. It is anatomically based and templated.
Trending article: How to integrate dental digital imaging with your paperless workflow
“It’s to keep dentists out of trouble,” he said. “It really is to reduce their risk of missing something in their scans because every manufacturer tells me one of the things doctors tell them is, ‘Wow. It’s doing great. I love the images I get, but I’ve got to learn more anatomy, and, by the way, I’m really afraid of missing something.’”
The software teaches doctors how to review a scan and shows them what’s important and what they must refer.
EasyRiter is available on the Dentrix Marketplace. Along with several articles about imaging, it is also available through Dr. Miles’ website at learndigital.net.
Changing daily duties
The greater accessibility of 3D imaging is changing how doctors work, providing better outcomes. As the machines make their way into practices, doctors are able to do much more.
“Over the years, I have used 3D imaging, but I found myself always referring patients out to scan centers for me to get that information,” said Dr. Dan Indech, DDS, a periodontist in Phoenix, Ariz. “I would get either a disc or a DICOM file. I really wasn’t able to manipulate the data as well as I would have liked to, but having that information allowed me to make critical decisions regarding jaw anatomy, primarily in my implant dentistry practice. It’s allowed me to make diagnoses on conditions I couldn’t have arrived at with 2D imaging or clinical examination. Recently, I installed a 3D scanning machine, and it’s taken me to the next level with regards to having the data and being able to manipulate it in a manner that allows me to eventually see what I’m looking for.”
Trending article: How to ensure the entire team is on board with technology
Three-dimensional imaging allows doctors to see what they couldn’t see before on 2D images.
“It’s like the difference between radio and television,” Dr. Flucke said.
For example, he notes the anatomical average for upper molars is a three-root structure. However, some patients have four roots, and that is not usually visible on a 2D image.
“You look at a 2D X-ray of that situation, and because of all your training, your mind can look at that and say, ‘Oh, I know what upper molars look like,’” he said. “And that’s all well and good until you get the one that has four roots, and the roots are kind of overlapped on the X-ray, and you can’t really tell that. Then your mind says, suddenly, ‘Oh, I’ve seen this before. It’s three roots.’ And then you get in there and start mucking around, and you’re like, ‘I wasn’t expecting this. Now what do we do?’ How do we back up a few steps and redirect?”
More doctors embrace digital imaging and making theirs and their patients’ lives better.
“Dentists are actually finally doing a little more due diligence and educating themselves about the various tasks it’s capable of improving in their office, and so the capability of having both 2D gray scale and 3D gray scale or color imaging is tremendous,” Dr. Miles said. “It crosses a lot of different tasks dentists do from endodontics to implant planning to obstructive sleep apnea to TMJ to ruling out of sinus problems when they mimic dental pain. The applications are very broad, and the technology is very simple and very sound at this point in time.”
Improved cases
Drs. Indech and Flucke share some experiences about how 3D imaging improved cases that would have been more difficult without those scans.
Dr. Indech recounts a case where an impacted tooth was in a different position than the 2D image revealed.
“A teenage patient was referred to me for an exposure of an impacted canine tooth, and, typically, we’d go off of PAs or panoramics,” he said. “Nine times out of 10, the cusp of the tooth is somewhere in the palate area, and we open the palatal tissue, find the tooth, expose the crown, attach a bracket and bring the chain out of the gum so then the orthodontist can pull the tooth into the mouth. In this particular case, I took the 3D image, and I could see from it (I couldn’t see this from the panoramic that the orthodontist sent me) that tooth was actually erupting on the facial side. In the past, I would have approached from the palatal side. I wouldn’t have found the tooth, and I would have had to open the facial side to eventually get the procedure done. In this way, we went straight to the facial side, found the tooth and attached the bracket, and it ended up being much less traumatic surgery for the patient. Going forward for exposures of impacted canines, I won’t do one without a CT scan just because of the possibility that it’s somewhere we don’t expect.”
Trending article: 5 technologies your practice needs to invest in now
At Dr. Flucke’s practice, a man had a bridge secured to teeth that needed replacement every couple of years. Not wanting to keep replacing the bridge, they decided to attach it to implants. The 3D scan showed the larger problem.
“When you take 2D, the pictures you get are if you’re looking straight on the teeth,” Dr. Flucke said. “The nice thing about 3D is you can pick things up and spin them around and look at them from any direction. Once you’ve got a 3D image, you can look at things front, back, top, bottom or whatever you can imagine.”
It turns out the roots of one tooth holding this bridge were tipped at an awkward angle.
“The upper teeth were tipped at this crazy angle,” he said. “The roots were going one way, and the bridge was going the other.”
The bridge was created to correct an underbite.
“The problem is the physics of that situation,” Dr. Flucke said. “The reason this bridge wasn’t working is because when he bit down, he was torquing the teeth around, and the teeth were breaking inside the bridge. You couldn’t see that at all unless you looked at the patient’s mouth sideways. Suddenly you saw it.”
Trending article: Top technologies for caries and cancer detection
It went from an implant case to something much more complicated.
“The time to realize the way things were was not when I was in the middle of doing the case because if you extract teeth and suddenly realize, ‘Oh, wait. This is all completely cockeyed and different, and we are going to have to do a bone graft,’ you don’t want to learn that once you’ve got the front teeth out. That’s a bad day,” Dr. Flucke said.
Future wishlist
As with any technology, 3D scanning will continue to evolve. What do doctors and labs want from the technology?
“In the specialist arena, you’re going see 3D cephalometric analyses start to be derived,” Dr. Miles said. “I think Dolphin and some of the imaging companies that started with the orthodontic community are still working toward that. Virtual articulators can capture the data with the teeth in separation but then mimic the movements from other data you get from a clinical exam. You don’t even need to have the patient there to see the animation and the true movements of the teeth together. So you’ll see that come along.”
Clausen anticipates more dental professionals will adopt the new technologies.
“I think the biggest changes will be in adoption rates,” he said. “You’ll see more and more professionals routinely using digital imaging. Every dental school will need to teach it and, as I said, professionals embrace it. It is simply a more efficient and better way to work.”
Whether or not 3D will completely supplant 2D images is up for debate, but Dr. Flucke believes 3D imaging will continue to grow in popularity.
“Intraoral scanners make it so much easier to do crown and bridge, and they’re just continuing to pick up steam,” Dr. Flucke said. “That’s the way it’s going to be for the foreseeable future. I don’t know if by the time I leave the profession that more than 50 percent of what we do will be digital. At some point in the not too distant future, this digital impression thing is going to wipe out impression material. There’s no doubt.”
Dr. Indech said those using 3D imaging find new and unexpected ways to use the technology, and those uses will continue to change.
“Endodontic diagnosis is a big area where we’re seeing things we could never see before and conditions that are challenging to diagnose,” he said. “Vertical fractures, perforation defects and lesions in bone are hard to see where they are, and now we can see them very clearly and come up with tighter treatment recommendations for those endodontically challenged. That’s a big area that I think will continue to grow, and there’s a big value for the periodontist because for those teeth that have continued to struggle with endo treatments and conditions, chronic pain and non-feeling infections, at some point the endodontist gives up and refers the patient to the periodontist. It’s easy to deal with those teeth by extracting them, but there’s a big value in having a visual record of what was actually wrong with that tooth should it come full circle at a later date as protection for the endodontist or myself.”
Rogers sees the future of 3D imaging as creating even better collaboration between different manufacturer’s components and systems.
“They’re kind of fragmented-all in their own independent silos,” Rogers said. “There’s not a lot of cross functionality among them. What I think you’ll see is, and that’s why Zahn and Henry Shein are excited to work with some of our partners, like 360imaging, is that we are able to create this workflow where the surgeon, restorative doctor and laboratory can take the CT of the patient and integrate it into a software like 360imaging’s DPS software, create a surgical plan with one of Zahn’s 3D printers like BEGO and actually print the surgical guide. Then they can make all of the restorative components, such as a custom implant abutment, and then a final restoration before surgery even happens.”
Trending article: The top advances in caries detection

So rather than have three or four office visits for the patient in your traditional analog workflow, you can reduce that treatment down to one or maybe two visits. That does a few things. It reduces the chairtime for the clinician, which increases his or her profitability, and allows the laboratory to handle the case prior to it coming through the door so they’re able to order all their parts and pieces prior. They’re also able to establish the lab bill’s cost up front for the restorative doctor so therefore they remain profitable.
“The patient has better treatment, and we provide them with the new standard of care with 3D imaging, 3D printing and all this cool stuff with guided surgery,” Rogers said.
Trending article: CAD/CAM: Having it all ... your way
The technology itself will progress, but Ferguson also notes how doctors and labs use it will evolve, as well.
“What I’m excited about is outside the new technology,” Ferguson said. “A cone beam can be done in 10-20 seconds or so, and, with the processing afterwards, you have a 3D image quickly, and it’s really accurate data. Using it for somebody’s mouth or jaw, what other uses can we have for this technology in terms of quality assurance in the restorative process, being able to see things we never saw before, fitting and manufacturing? I relate it back to when we first started doing CAD/CAM in the dental field, and all of a sudden we could vary the translucency of an opposing arch and really see areas of the crown we were designing that we were never able to see before because we had a stone model that was in the way. What doors is this going to open now that we can see even more things?”
Cost
Cost is, of course, an issue for any practice considering 3D imaging. Dr. Indech has advice for those contemplating such a purchase.
“I look at it in two ways,” he said. “In a more narrow manner, I want to know I’m utilizing that piece of equipment sufficiently to cover the investment I made. But, on a broader basis, I take a look at where we’re going, where we’re at with standard of care and the value to me with having that information both from a diagnostic and protective standpoint. You really can’t put a price or a number on it, and what I found in the short amount of time I had my own machine is there are cases I previously couldn’t do, but once I got the data and analyzed it, I decided I could do them, which increased the number of cases that get into my schedule. On the other hand, there are cases I may have looked at with other forms of data, 2D panoramics or PAs, and I may have opted to do them, but once I evaluated the scan information, I decided either not to do them due to risk or to treat them differently.”
Trending article: A change whose time has clearly come
Price is an issue, but, like any popular technology, advances and vendor competition are likely to make machines more affordable.
“It’s still pretty pricey, but there’s so much competition, and as it whittles down, newer companies are going to be bringing things to the table,” Dr. Miles said.
Ultimately, 3D imaging has a profound impact on the dental profession and it is worthwhile for doctors to consider when or even if they will add the capabilities to their practices.
“The office of the future is going to have one or two portable/handheld X-ray generators,” Dr. Miles said. “You could have it on a portable arm and just move the tube head around where you need it so there’ll be portable X-ray generators and a panoramic on steroids, meaning they have more functionality. And then there is cone beam. Cone beam is either ‘I need it, I have to have it and I can make it work,’ or ‘I only need the data from it, and I can get it from a lab, friend or a mobile and use that data to do the things that I want to do.’ So there’s really no need for a dentist who doesn’t want to extend the capital to actually buy it for his or her office, but I believe everybody’s going to either use it in their office or data from an office that has cone beam to make better clinical decisions.”
“2016 promises to be a great year,” Clausen said . “The majority of labs don’t feel threatened by digital technology anymore. They recognize it is making their job easier, increasing productivity and enabling them to provide new product offerings. Practices are warming up, as well. The doctors who have converted to digital will never go back.”
Collaboration
Technological advances have made the task of communication and collaboration between team members much easier and more streamlined.
“I believe 3D imaging has dramatically changed the way doctors and labs work not necessarily in the type of service they offer, but in how they perform their job,” Clausen said. “In labs, on a very basic level, you could say the mouse has replaced the traditional wax-sculpting tool. We have always considered labs and practices to be part of the same team. Digital technology has served to improve their ability to work closer together and achieve better patient outcome.”
Trending article: Dr. Flucke's insights on CAD/CAM technology

CBCT scans provide a great amount of detail for the patient’s entire head and not just the teeth. This information is useful for all members of the team to produce the best results.
“You can have input because you can communicate this data clearer, sharper and more concisely between the surgeon, restorative doctor and laboratory,” Rogers said. “So you can really predict not only the surgical outcomes but also the restorative outcome prior to anything really happening with the patient.”
Collaboration does not have to be done in-person. Thanks to digital imaging, the scans can be shared, virtually, with members of the team meeting from different locations.
“If you’re in, for instance, what I like to call the mythical place, ‘Small Town, Ark.,’ and you’re the only dentist for 100 miles, the nice thing about it being all-digital is you can have someone drive to Little Rock to the best implant surgeon in the state and do a group meeting where you share your desktop” Dr. Flucke said. “You can sit down with a colleague who you may have never met face to face before, and they could actually see the exact same thing in a sit-down meeting.”
“These more complex cases are becoming less and less complex because you’re allowing each team member of the restorative process to collaborate and give the best outcome for the patient at the end,” Ferguson added.
Trending article: How a small piece of technology made a huge difference in one dental practice
Surgical guides
Because CBCT scans reveal bone structure in addition to dentition, they are ideal for preparing dental implant cases. Labs are able to use those scans to create surgical guides that make the process of drilling pilot holes easier and safer.
Performing implant cases freehand is, of course, possible, but utilizing a surgical guide can help prevent unwanted outcomes.
“I’ve reviewed more than 18,000 cone beam scans from all the different machines and manufactures and my clients,” Dr. Miles said. “The number of implants I find that are not in appropriate locations is somewhat startling, and I can almost state, without any hesitation, that those implants that I find in unusual locations, the practitioner did not use a surgical guide. Had they used a guide, they would have been in the appropriate location. I see lack of bone over the facial or the outside aspects of implants. I see implants in the sinus. I see implants in the nasal cavity.
“I would think that our profession, in the next 10 years, is probably going to move toward almost every implant being placed using the surgical guide of some description,” Dr. Miles said.
So if you’re into implants, this technology is a must. And even if you’re not, the benefits from this technology will continue to grow, and so will its use.