How to improve patient care with laser dentistry
One clinician describes the advantages offered by the Ultradent Gemini soft tissue laser.

When I first saw the Ultradent Gemini laser in its development, it did not have all of its corporate logos, but it stood apart from all other lasers in its appearance with its electroluminescent display. It draws you in to learn more about it and it delivers. This laser has so many features, but I will only highlight some of the most clinically relevant.
Two features that set the Gemini apart is that it can deliver two wavelengths simultaneously and do so with 20 watts of peak power delivered in a super-pulsed mode. For years, the debate has been which soft tissue diode laser wavelength is the best to use, with the two common being the 810 nm and 980 nm. The 810 nm wavelength laser energy is best absorbed by pigmentation in the tissue provided by hemoglobin and melanin, while the 980 nm wavelength energy is absorbed more by water. The Gemini can deliver each wavelength individually or both simultaneously, which is genius.
Trending article: Technology evolution and the Gemini laser
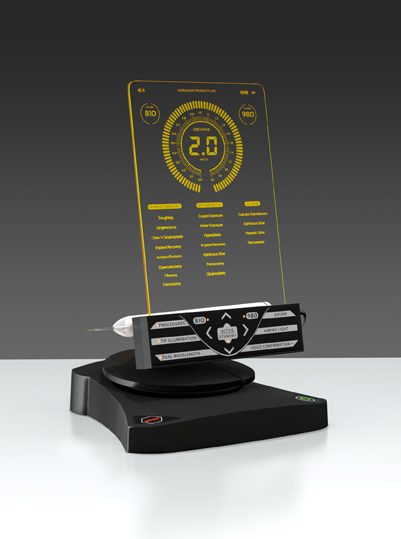
And it gets better with the 20 watts of peak super-pulsed power. This means that to deliver an average power output of 2 watts (more, than twice what I would typically use) the Gemini only needs to be active 10 percent of the time, allowing for thermal relaxation or tissue cooling, and the result is greater patient comfort and smoother, faster tissue ablation.
I have used soft tissue diodes lasers in my practice since the 20th century because of the predictability it affords me and the comfort my patients experience. Better-fitting crowns without the need to pack cord, excisions without prolonged bleeding, frenectomies without the need for sutures-the list of advantages goes on. Telling a patient we are going to use a laser to “vaporize” the tissue to create the ideal smile or fabricate a better-fitting crown sure beats having to tell a patient you are going to “cut off” the tissue with a blade and then help them manage the bleeding and pain afterward.
I have the privilege of talking with clinicians around the world about lasers, and I find that there are often three main concerns in considering their adoption of a soft tissue diode laser in their practice. The first concern is the cost, the second is finding the need in their practice, and, lastly, they ask about the learning curve and education needed.
Trending article: Choosing a dental laser for your practice
The investment
When discussing the cost, I think of a laser as more of an investment. It will return to you the actual cost of the laser and be a continued source of revenue. And it will change your patients’ perception of your practice, making it a powerful marketing tool. But these are the business benefits; clinically, I feel you are able to treat your patients better with a laser and that is what truly makes it priceless. It should be remembered that when it comes to reimbursement, we are reimbursed for the procedure performed, not the specific technique used. Whether we perform a gingivectomy with a surgical blade or a laser, it makes no difference, provided the service was indeed done. The concern about the cost of the laser must be tempered by the revenue it will generate, and the savings in time and material.
Continue to page two for a case study.

The need
If you do crowns, place subgingival fillings, or treat patients for periodontal disease in your practice, the need is there. Let’s review some of the uses of the Gemini laser and see how easy it is.
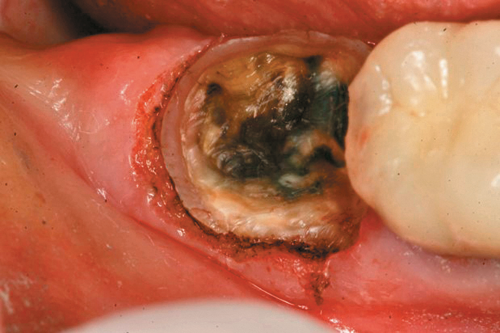
Figure 1 shows an example of a deep subgingival margin with the ensuing bleeding. If we are planning on packing a cord, we need to pack multiple cords soaked in hemostatic agent and wait for the soft tissue to move away from the tooth margin and achieve hemostasis. We have all experienced the moment of truth when the cord is removed, which oftentimes reinitiates the bleeding and the soft tissue again flops over the tooth margin, making it almost impossible to get an adequate impression the first time. This results in the loss of time, incurred cost of another tray full of material and the patient needing to undergo a mouthful of gagging material.
Related reading: Ultradent introduces Gemini 810 + 980 soft tissue laser
Compare this to use of the Gemini laser. We can set the power setting of the laser using the preset power settings for “Troughing” (Fig. 2) at 1.1 watts. The pre-initiated tip (pigment on the laser fiber converts some of the laser energy to photothermal energy) is placed into the sulcus to ablate the soft tissue, which creates a clear separation of the soft tissue from the tooth margin and achieves instant hemostasis (Fig. 3). We then have no need to wait and can immediately take the impression (Fig. 4). I consider this alone as priceless in my day-to-day practice.
This example of using a laser is one that saves me time and material, but this is not a procedure that carries with it a fee unless you charge to pack cord. The next few clinical examples show the use of a laser, and each of these would be charged out the same as if you had used a surgical blade or an electrosurgery unit, but often the patient will not have to endure an injection of anesthetic or wait for healing and return for multiple visits, thus creating the ideal win-win situation for our practice and patient.



Fig. 1 Fig. 2 Fig. 3
Smile design
I think the use of soft tissue lasers in a smile design case demonstrates the predictability of healing in the esthetic zone, where we often have thin tissue and exact margin placement. When working on a smile design case, we want to achieve symmetry of the gingiva, and position the height of the soft tissue of the cuspids and central incisors evenly and 1-1.5 mm above that of the lateral incisors, with the gingival zenith positioned slightly distal to the midline of the teeth to help create the appearance of their mesial inclination.
Fig. 4
To see the value of using a soft tissue diode laser, let’s look at the alternatives such as a surgical blade procedure or using an electrosurgery unit. With both these options, we need to administer an injectable local anesthetic. Using a blade, our patient will have postoperative bleeding and discomfort to manage, and we have to wait for the tissue to heal before we prepare the teeth and take a final impression. Alternatively, if we used an electrosurgery unit, we would not have the postoperative bleeding, but we would still need to wait for the tissue to heal before preparing the teeth because of tissue necrosis.
Trending article: How Genius Endo can simplify endodontics
With a soft tissue diode laser, we can often recontour the tissues after the simple application of a topical anesthetic, such as Ultracare, a 20% benzocaine gel. Using Ultradent’s Gemini soft tissue diode laser, we can select the preset power setting for “Gingivectomy” at 1.2 watts and wipe the tissue away. I have my assistant blow air on the area and hold the high volume evacuator close to remove any heat, which is the only sensation the patient might feel. Done properly, we will not see any significant changes after tissue healing.
Here is a case where the tissue has been recontoured before veneer preparation (Fig. 5), and during this same appointment the equi-gingival veneer preparations were finished and impressions were done. A few weeks later the veneers were placed and Figure 6 shows the predictability in tissue position.


Fig. 5 Fig. 6


Implant recovery
When it is time to uncover an implant body, I use Ultradent’s Gemini laser in the “Implant Recovery” setting at 1.5 watts. We place Ultracare 20% bezocaine on the tissue for a minute and then “wipe” the tissue away until the implant body is exposed sufficiently (Fig. 7). The implant doesn’t absorb the laser energy being metallic and there is not the sparking seen with an electrosurgery unit.
Trending article: 5 ways composite advances can change your workflow
Biospy
This patient presented with a benign growth of hyperplastic tissue due to irritation from a removable partial denture. This was caught during her prophylaxis appointment and its removal was as simple as placing Ultracare 20% benzocaine topical anesthetic for a minute, placing the tissue under tension by having my assistant pull the tissue with tissue forceps while I ablated the tissue at its attachment (Fig. 8a-c). We used the “Incision/Excision” preset, which delivered 1.2 watts. When sending the sample for biopsy, one must specify how the sample was collected, which in this case was with the laser as the pathologist may see the heat artifact and needs to understand why it is present.


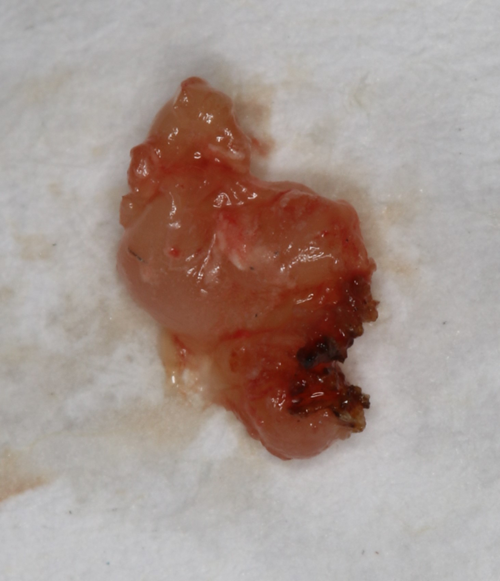
Fig. 7 Fig. 8a Fig. 8b
Hygiene
An area where lasers can often be used is in hygiene care by hygienists (check with your local State Board to determine what services hygienists can legally perform). The hygienist can use the laser to disinfect the sulcus and treat necrotic tissue in non-healing pockets. Using the Gemini laser, we go to the hygiene preset “Sulcular Debridement,” which gives us 0.4 watts of power now with a 7 mm non-initiated tip, and gently wipe the tip through the sulcus to warm it up 60Ë C and disinfect the sulcus. After root planing and scaling, we initiate the tip and treat the necrotic tissue in the sulcus (Fig. 9). One nice feature of the Gemini is the illuminated tip, which aids in the visualization of the tissue in the difficult to see areas of the oral cavity.
Trending article: 5 reasons to revisit lasers for your dental practice
Education
I have reviewed many different procedures that can be accomplished with Ultradent’s Gemini soft tissue laser and there are so many others, such as the treatment of aphthous ulcers, frenectomies and so many more. The patient benefits are the main driver for me using the laser and making the investment. The last concern I mentioned in the beginning was the training and education. Fortunately, as you can see from the cases shown, the use of the laser is very easy and safe, and with the Gemini laser, Ultradent will help you with live certification courses, online training and shorter introductory course training. Ultradent wants your laser experience to be successful and safe.
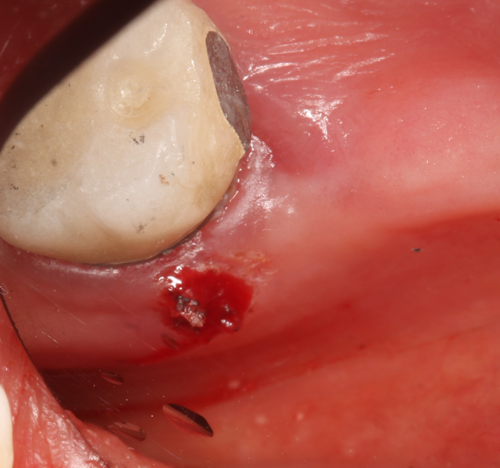

Fig. 8c Fig. 9
Conclusion
I encourage doctors to join the 21st century and see how a laser can positively impact their practice; given a chance, I know it will. And best of all the use of the Gemini will be appreciated by the your patients with the need for fewer visits and amazing treatment outcomes.
