How to achieve both retention and prevention with BioCoat
Why this sealant should be added to clinicians’ caries management armamentarium.

Sealants are one of the most effective preventive procedures we can offer to our patients.1 With proper placement, sealants have proven efficacy and can provide a protective barrier for the occlusal surface of the tooth against decay. Dental sealants are esthetic and noninvasive, they don’t require local anesthesia, and they can be a cost-effective method for prevention of caries. However, dental sealants are still underutilized, as the Centers for Disease Control and Prevention estimates that the prevalence of sealants in the United States for children ages 6-11 is 43.2 percent.2
Tooth decay is largely preventable via appropriate oral hygiene and diet, but it remains one of the most common diseases of childhood - five times as common as asthma and seven times as common as hay fever, according to the American Dental Association.3,4 Because of this, oral healthcare professionals (OHCPs) should always be looking to add new, effective tools to their caries management armamentarium.
Trending article: How bioactive materials are changing restorative dentistry
Choosing a sealant: retention or prevention
When choosing a dental sealant, clinicians have several factors to consider, including retention, durability, strength, flow, ease of use, esthetics and if it offers fluoride release for added protection. Modern pit and fissure sealants are typically resin-based or glass-ionomer-based (GI). Resin-based sealants are stronger and offer better retention, whereas GI sealants are more soluble but may offer additional prevention because of fluoride release.5,6 So, the dilemma for OHCPs involves choosing retention or prevention when selecting their dental sealant material.
Resin-based sealants are sometimes additionally classified as either containing glass filler (filled) or not containing glass filler (unfilled). Fillers are present to provide hue, strength and added wear resistance by increasing shear bond strength and compressive strength. But too much filler can affect the handling of the material. Sealants have to be “thixotrophic,” meaning that as shearing force is applied by expressing the material through a metal cannula, it lowers viscosity. This is essential to help create a sealant that easily flows into pits and fissures, with or without manipulation.6,7
Most resin sealants are hydrophobic and need to be placed in a dry field, but this also helps make resin-based sealants less soluble and highly retentive. Resin sealants typically have a wide range of characteristics, including several color choices and varying means of polymerization (light-cured, dual-cured). Resin-based sealants are also associated with better retention rates compared to GI sealants.
Glass ionomer sealant materials are composed of an aqueous solution of polyacrylic acid that reacts with calcium fluoro-aluminosilicate glass powder.8 The glass powder creates the potential for fluoride release; however, because fluoride is part of the material’s matrix, this also contributes to solubility in the oral environment. GI sealants are more hydrophilic compared to resin sealants and can be suitable for placement in a moist (not wet) environment and are specifically indicated for partially erupted teeth or as interim sealants.5 Because the strength of GI materials is lower than that of resin sealants, and combine that with higher solubility, GI sealants can be less retentive.5,6
So, what do you choose: retention or prevention? What if there was a sealant that offered both?
Read more: I Use That: BioCoat
Bioactivity and remineralization
The term bioactivity when applied to dental materials has been defined as: “the property of a biomaterial to form apatite-like material on its surface when immersed in a simulated body fluid (SBF) for a period of time.”9 So, the fluoride released from a dental material is really more “bio-available” because in order to form calcium fluorophosphate (aka fluorapatite), there must be calcium and phosphate present.
The availability of calcium and phosphate in the remineralization process is essential. Although fluoride serves as a catalyst for remineralization, it will not occur unless adequate amounts of calcium and phosphate ions are available.10
When fluoride, calcium and phosphate ions are present, the ions can help prevent carious lesions, limit the progression of carious lesions and enhance the repair of early lesions already present by promoting remineralization and preventing demineralization.
Up next: BioCoat with SmartCap Technology...
BioCoat™ with SmartCap™ Technology
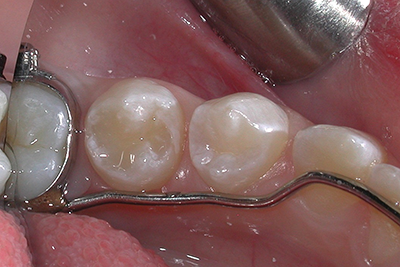
Now, OHCPs can have the best of both worlds, a sealant that is both retentive and preventive. Premier Dental introduced BioCoat™, a bioactive resin pit and fissure sealant, to offer both the retention of a resin-based sealant and the fluoride release of a GI (Fig. 1). BioCoat™ releases not only ionic fluoride but also ionic calcium and phosphate.

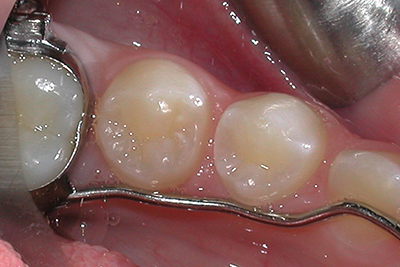
Fig. 1 Fig. 2
SmartCap™ Technology, developed through a partnership with Premier Dental and Creighton University School of Dentistry, incorporates patented semi-permeable resin microcapsules. In BioCoat™, the rechargeable SmartCap™ microcapsules are filled with ionic solutions of fluoride, calcium and phosphate, which continuously diffuse in and out of the sealant. The ions supersaturate the oral environment around the enamel, which provides defense against demineralization during acid attacks.11 The daily release of remineralization ions provides long-term protection while strengthening enamel and sealing margins against microleakage. There’s no degradation of the restoration matrix resulting from the fluoride release, as is possible with glass ionomers. And SmartCap™ microcapsules are truly rechargeable. When exposed to saliva and normal tooth brushing, the SmartCap™ microcapsules can absorb fluoride, calcium and phosphate to prolong the protection.
Trending research: Does water fluoridation actually prevent tooth decay?
Technique tips for optimum sealant retention
Retention of dental sealants is essential to their effectiveness in caries prevention and is often impacted by clinical skill, technique and control of the oral environment. Each sealant manufacturer has specific directions for use of their sealant material and following these instructions is critical for the success of sealant placement.
Directions for the placement of BioCoat™12:
1. Attach dispensing tip to BioCoat™ syringe.
2. Clean fissures using oil-free pumice, air polishing prophylaxis system, or thin diamond fissure/prep bur (Figs. 2-4).


Fig. 3 Fig. 4
3. Isolate teeth being treated to avoid saliva contamination.
4. Apply etch to fissures for 20 seconds. Thoroughly rinse and dry. If using sodium bicarbonate in air polishing system, repeat with a 5-second etch, then thoroughly rinse and dry (Figs 5-7).


Fig. 5 Fig. 6
5. At initial use, express a small amount of BioCoat™ onto a mixing pad prior to applying intra-orally.
6. Slowly introduce BioCoat™ into the pits and fissures. Do not let the sealant flow beyond the etched surfaces and avoid pooling. An explorer tip may be used to direct the flow and ensure that all pits and fissures are sealed (Fig. 8).


Fig. 7 Fig. 8
7. Light cure with a dental curing light (of no less than 600mW/cm2) for 20 seconds. The tip of the light guide should be held as closely as possible to the sealant without actually touching it.
Read more: Premier Dental launches PremierAir product line
8. Inspect the sealant for complete coverage and to prevent voids.
Fig. 9
9. After confirming placement, wipe the sealant with a cotton pledget to remove the air-inhibited layer (sticky surface after curing) and check occlusion. Adjust as necessary (Fig. 9).
Conclusion
While dental sealants are a proven strategy in the caries prevention armamentarium, many studies report that sealants are underutilized. With “CAMBRA” protocols, sealants aren’t just for children. Sealants should now be placed based on caries risk and not age, so they may be indicated for adults as well.13 When selecting a dental sealant, there’s now a material that offers the retention expected from resin but also the remineralizing ions needed for prevention - Premier Dental’s new sealant, BioCoat™ with SmartCap™ Technology.
References
1. Wright JT, Crall JJ, Fontana M, et al. Evidence-based clinical practice guideline for the use of pit-and-fissure sealants. J Am Dent Assoc 2016;147(8):672-8.
2. Vital Signs: Dental Sealant Use and Untreated Tooth Decay Among U.S. School-Aged Children. Centers for Disease Control and Prevention. October 21, 2016. Available at: https://www.cdc.gov/mmwr/volumes/65/wr/mm6541e1.htm. Accessed April 22, 2018.
3. Benjamin RM. Oral health: the silent epidemic. Public Health Rep 2010;15(2):158-9.
4. Frequently asked questions on community water fluoridation. American Dental Association. Available at: https://www.ada.org/~/media/ADA/Public%20Programs/Files/Fluoridation_FAQs.pdf?la=en. Accessed April 22, 2018.
5. Crall JJ, Donly KJ. Dental sealants guidelines development: 2002-2014. Pediatr Dent 2015;2:111-5.
6. Condo R, Cioffi A, Riccio A, et al. Sealants in dentistry: a systematic review of the literature Oral Implantol 2013;6(3):67-74.
7. Munoz HE, Silva JC. Pit and fissure sealants: an overview. 2013. PennWell Publishing. Available at: https://www.rdhmag.com/content/dam/rdh/print-articles/Volume%2033/Issue10/1311cei_Mun%CC%83oz_RDH_7.pdf. Accessed April 22, 2018.
8. Smith DC. Composition and characteristic of glass ionomer cements. J Am Dent Assoc 1990;120(1):20-22.
9. Jeffries SR. Bioactive denal materials. Inside Dentistry 2016:12(2). Available at https://www.aegisdentalnetwork.com/id/2016/02/bioactive-dental-materials. Accessed April 22, 2018.
10. Reynolds EC. Calcium phosphate- based remineralization systems: scientific evidence? Aust Dent J 2008;53:268-73.
11. BioCoat™ Part 1 Technology. Premier Dental Products Company. Available at: https://www.premusa.com/wp-content/uploads/2017/04/biocoat_technical-guide_PART1_R1.pdf. Accessed April 22, 2018.
12. BioCoat™. Available at: https://www.premusa.com/product/hygienepreventative/biocoat/. Accessed April 22, 2018.
13. Hurlbutt M. CAMBRA: Best practices in dental caries management. 2011. PennWell Publishing. Available at: https://www.rdhmag.com/etc/medialib/new-lib/rdh/site-images/volume-31/issue-10/1110RDH095-109.pdf. Accessed April 22, 2018.