Different Ways to Protect Dental Pulp
We explain the options for lining cavity preps to protect the tooth structure and the advantages and disadvantages of each.
Different Ways to Protect Dental Pulp. Photo by Alexandr Mitiuc/stock.adobe.com.
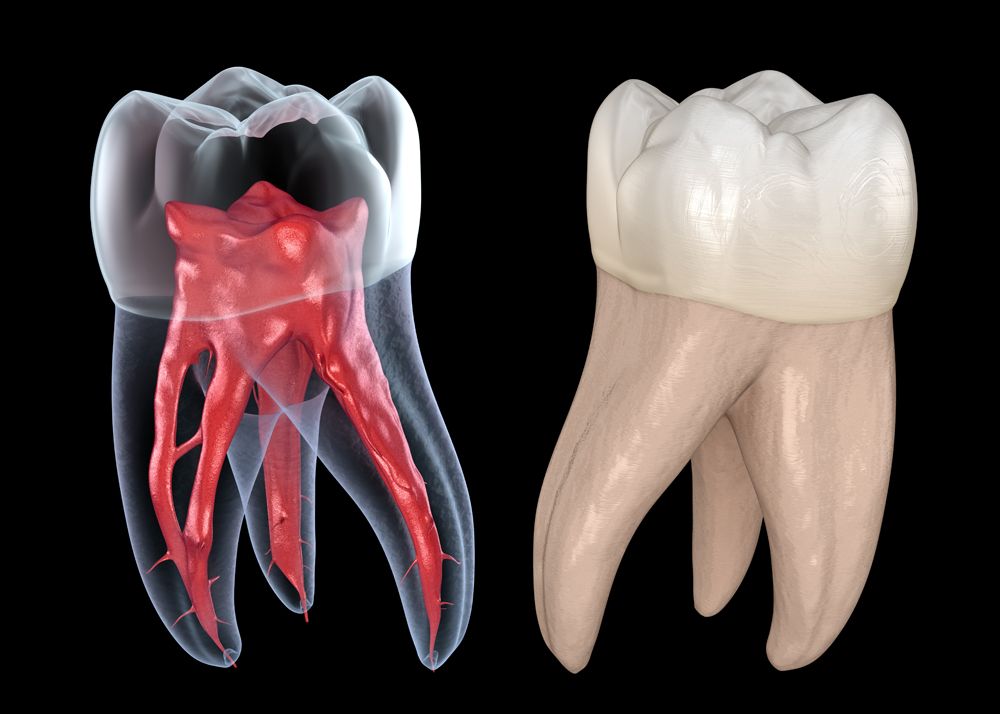
Protecting the pulp is essential when it is exposed in preparations to prevent pain, infection, and the eventual loss of the tooth. Pulp capping can help, which involves sealing materials over the exposure to protect the pulp. There are many options for pulp capping in restorations. We take a closer look at some of them and the newer players in the field that can serve this essential function in your restorations.
There are a few ideal qualities for pulp capping materials. No matter which material you choose for protecting the pulp, the Journal of Pharmaceutical Sciences and Research (JPSR) suggests it should be bactericidal or bacteriostatic, sterile, and radiopaque. Also, it should also:
- Stimulate reparative dentin formation
- Maintain the pulp vitality
- Release fluoride to prevent secondary decay
- Adhere to restorative material
- Resist forces for longevity
In addition, the JPSR says some common materials pulp capping materials include:1
- Calcium Hydroxide
- Glass Ionomer Cement
- mineral trioxide aggregate (MTA)
- Biodentine
- Castor Oil Bean
- TheraCal
- Propolis
A literature review appearing in Operative Dentistry in 2009 has the following advice for successful pulp capping:2
- Start by avoiding pulp exposure in your preparation, even if it means residual caries remain behind, to increase the chances of tooth survival.
- Control bleeding with water, saline, or sodium hypochlorite as they will be gentle with exposed pulp, and sodium hypochlorite can disinfect the area.
- Avoid Glass Ionomers and Resin-Modified Glass Ionomers, and adhesives for pulp capping because of their poor performance.*
- Consider using MTA as it produces comparative results to Calcium Hydroxide.
- Use Calcium Hydroxide for direct pulp capping because of its long track record of success.
- Seal the restoration well right after pulp capping to protect against leakage and bacterial contamination.
*An in vitro study in 2018 demonstrated that light curing pulp capping materials caused deformation of pulpal dentin and increased pulpal temperature in large mesio-occlusal-distal (MOD) bur preparations with 1mm of dentin remaining at the pulp floor. There was no difference between the 3 materials for preventing the pulpal temperature increases.3
The Latest and Greatest in Pulp Protection
However, much has changed in the materials for pulp capping over the last decade or so. While Calcium Hydroxide remains effective, other materials might challenge its gold-standard status and last longer. Tim Bizga, DDS, FAGD, a private practice dentist outside of Cleveland and lecturer for the dental industry likes using different materials in his liners for pulp protection. He is a big fan of BISCO’s Thera line products that use calcium silicates in their formulation.
TheraBase™ is a dual-cured product that releases calcium and fluoride after placement. The self-adhesive base or liner creates an alkaline PH, which is designed to promote pulp vitality. In the Bisdent Globe newsletter, one doctor describes it as forming “a protective barrier that insulates the pulp.”4
One of the other products in BISCO’s line is the TheraCal LC®, a light cured flowable resin-modified calcium silicate liner. It contains MTA and is designed to be a pulp cap for direct and indirect restorations.
A Deeper Dive on MTA
MTA is made up of tricalcic silicate, tricalcic aluminate, and bismuth oxide and is a biocompatible material. MTA is made up of fine-sized particles that are hydrophilic and harden in the presence of dampness or blood. MTA is also radiopaque and harder to infiltrate than other materials used for the same purpose. In addition, MTA hardens slower than other materials (in a range of about 2 hours and 45 minutes to 4 hours), which reduces the tension internally on the restoration. Moreover, MTA has a reputation for superior sealing properties, which makes it excellent for many purposes, including protecting exposed pulp in preparations.5
Dr Bizga likes how the BISCO materials with MTA are light-curable, which means you can set the material immediately. Most MTA materials require a couple of hours to set, which doesn’t work for clinicians in a busy practice setting.
“What is really great about BISCO’s MTA materials is they release a ton of calcium, and they tend to skew toward the pH Alkaline scale. So, when you put them in deep dentin or an area where you’re concerned that the pulp will be irritated, this has unique chemistry that helps,” Dr Bizga says.
Research from Contemporary Clinical Dentistry suggests that MTA and TheraCal support the formation of tertiary Dentin, which is reparative dentin. However, the authors also suggest that because TheraCal has an easier application, improved sealing ability, and allows for permanent restoration placement in the same appointment, TheraCal is recommended as an alternative to MTA.6 Dr Bizga likes how it counteracts decay and creates a pH alkaline environment inhospitable to bacteria.
“You’re killing the bacteria with an alkaline environment, which allows the body to self-repair and heal,” Dr Bizga explains, adding that these products begin to cross over into biodynamic materials.
Some clinicians would rather use a glass ionomer, and Dr Bizga thinks that is great for many cases. However, in deep preparations, the way glass ionomers set can be an irritant to pulp. This situation pushes restorative dentists toward alkaline pulpal protectants.
“If they are alkaline, the pH scales differences are more calming to the tooth than irritating. It’s the thought process about where you are and how it changes the materials you use,” Dr Bizga says.
One of the other things Dr Bizga likes about these liners is that it replaces the 2-step process required when using calcium hydroxide covered by glass ionomer. Depending on the patient or the productivity targets, many clinicians may not want a 2-step liner process. He thinks that all of the calcium silicates liners are quicker to place and have the same properties as the historical liners that came before. What you choose depends on the case and what you are trying to do, and even whether to line it at all.
“It’s clinician’s choice,” Dr Bizga says. “I have been in rooms with KOLs who say your restoration is only as strong as your weakest link. With that thinking, clinicians might think, ‘Why am I putting on a weakly-bonded material at the bottom of the restoration that could potentially undermine it?’”
Dr Bizga says there are 2 schools of thought on lining. Some clinicians describe it as a coverup for poor bonding technique; others see it as a way to add a material that can help the tooth as much as possible with ion release in the area, even if it requires another step. Dr Bizga uses a case-by-case basis for his liner placement, seeing them as a tool for specific restorations rather than a typical step in all his restorative treatments.
“I make a judgment call based on what I see and what I think is going to be best to help the tooth and its life cycle,” Dr Bizga says. “It’s a great thing to have in your repertoire and the new lines available make placing them more convenient. And the science supports that they work.”
Getting the Most Protection with Your Liners
When it comes to placing liners, in addition to choosing the cases that require them, Dr Bizga has a few tips. Liners are best used sparingly, half-millimeter increments, as specified in the directions. The exception are bases because they are intended to go in thicker. Also, Dr. Bizga likes to disinfect the Dentin before placing any liner material down. Sometimes he uses a four percent chlorohexidine solution first; others he uses FiteBac® Antimicrobial Cavity Cleanser, which is a quaternary ammonium linked to polymerizable silane.
“It makes sense to me,” Dr Bizga says about disinfecting the tooth before placing a liner. “Any time you are applying some sort of paint, adhesive, or primer, the directions always say to get the substrate as clean as possible. While the bur does part of it, there is a microscopic level. This category helps make those protections better because if you are cleaning up the surface and then sealing that clean surface up, it gives the liner an even better chance of doing its job.”
References
Chandrasekhar H, Sharma S. Efficient Agents for Pulp Protection: A Review. Jpsr.pharmainfo.in. Published 2016. Accessed October 12, 2021.https://www.jpsr.pharmainfo.in/Documents/Volumes/vol8Issue11/jpsr081116014.pdf.
Hilton TJ. Keys to clinical success with pulp capping: a review of the literature. Oper Dent. 2009;34(5):615-625. doi:10.2341/09-132-0
CJ Soares, MS Ferreira, AA Bicalho, M de Paula Rodrigues, SSL Braga, A Versluis; Effect of Light Activation of Pulp-Capping Materials and Resin Composite on Dentin Deformation and the Pulp Temperature Change. Oper Dent 2018; 43 (1): 71–80. doi: https://doi.org/10.2341/16-325-L Accessed October 12, 2021.
Child, Jr. DMD, CDT P. Theracal LC—Over 5 Million Restoration Later: Are You Getting The Most Of It?. 1st ed. Chicago: BISCO; 2015:3. Accessed October 12, 2021. https://www.bisco.com/assets/1/7/MC-51160BD.pdf.
Casella G, Ferlito S. The use of mineral trioxide aggregate in endodontics. Minerva Stomatol. 2006;55(3):123-143.
Menon NP, Varma BR, Janardhanan S, Kumaran P, Xavier AM, Govinda BS. Clinical and radiographic comparison of indirect pulp treatment using light-cured calcium silicate and mineral trioxide aggregate in primary molars: A randomized clinical trial. Contemp Clin Dent. 2016;7(4):475-480. doi:10.4103/0976-237X.194109