Can root canal treatment be improved with prefabricated blood vessels?
Endodontic treatment is an effective option for patients whose dental pulp has become inflamed or infected. However, one of the major drawbacks of root canals is that the infected dental tissue is removed and replaced with synthetic biomaterials, which eliminates the tooth’s blood and nerve supply.
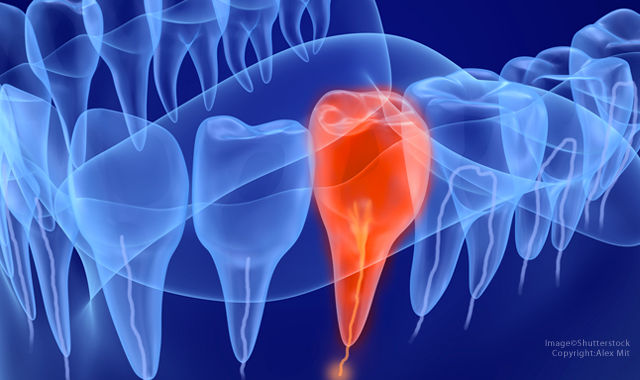
Endodontic treatment is an effective option for patients whose dental pulp has become inflamed or infected. However, one of the major drawbacks of root canals is that the infected dental tissue is removed and replaced with synthetic biomaterials, which eliminates the tooth’s blood and nerve supply.
With this in mind, researchers at the Oregon Health and Science University in Portland, Ore., developed a process to engineer prefabricated blood vessels in teeth. To do so, they employed a full-length root canal model wherein they fabricated a microchannel in cell-laden GelMA hydrogel tissue constructs. The researchers tested various concentrations of GelMA hydrogels and determined that the stiffer, 15% gels led to a higher rate of cell proliferation than softer gels.
Related research: New discovery could eliminate infections after root canals
To replicate a clinical situation, the researchers used extracted, endodontically-prepared, single-rooted human pre-molars and positioned an agarose fiber across the entire length of the root canal. They then loaded a cell-laden, 15% GelMA hydrogel precursor up to 3 mm of the root length and exposed the tooth to UV light for 30 seconds. They repeated the process three times to ensure thorough photo-polymerization of the material along the entire root canal. After seven days, the researchers discovered that dentin-producing cells proliferated near the tooth walls and artificial blood vessels formed inside the tooth.
"We truly believe that the strategy that we proposed can be an important step in replacing conventional root canal treatment methods with newer methods that are regenerative-based," states Luiz Bertassoni, DDS, principal investigator and an assistant professor of restorative dentistry at the OHSU School of Dentistry. "Much work remains to be done, but we hoped to illustrate that we can combine recent advances in biomaterials development, tissue engineering and stem cell biology to bring the idea of dental pulp tissue engineering closer to a clinical reality.
"Much work has already been done in this area with great success," Bertassoni continues. "But there is a great need for strategies that combine all of the knowledge that we have gathered over the years, with methods that can actually be done in the clinical practice by the clinician. Our method attempts to do just that. And we were able to show that using a set of skills and materials that can be easily translated into the dental clinic, we can achieve regeneration of vascularized dental-pulp like tissues. This is just the beginning, but our ultimate goal is to enable complete and reproducible dental pulp tissue engineering in adult patients as a gold-standard treatment, which means that the conventional treatment with Gutta-percha may become obsolete, and both the skillset and clinical requirements to perform these treatments may evolve as well."
Despite the results, the researchers pointed out a few limitations. They note that their proposed method does not reproduce the presence of other important tissue components, including nerves, fibroblasts and undifferentiated stem cells. In addition, they utilized cells isolated from different animal species, which they note may not be consistent with the behavior of human dental pulp cells.
“Despite these obvious limitations, we are convinced that the engineered microchannels could enhance the formation of cell-based microvessels in a hydrogel loaded with co-cultures of endothelial cells and dentin progenitor cells of human source,” the researchers state. “This forms the basis for future studies in our laboratory, as well as a more thorough in-vivo analysis of the effectiveness of the proposed approach.”
The study, titled “A Novel Strategy to Engineer Pre-Vascularized Full-Length Dental Pulp-Like Tissue Constructs,” appeared in the scientific journal Nature.