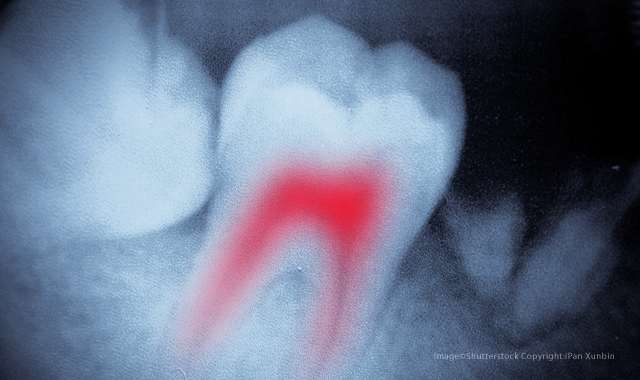
New discovery could eliminate infections after root canals
The new method of detecting bacteria during root canal treatments could eliminate secondary infections and the need for follow-up visits.
Root canals are bad enough without the threat of secondary infection and multiple follow-up visits. Now, thanks to a new device, researchers believe they can eradicate the need for numerous appointments-and cut down on treatment failure.
Since approximately a quarter of root canals fail over time due to secondary infections, the ability to detect potentially hazardous leftover bacteria at the time of treatment could be extremely beneficial. It could also cut down on the number of visits, as most procedures currently require one or two secondary visits to the dentist. The new device, called SafeRoot, was created to detect any remaining bacteria at the completion of root canal treatment to reduce the need for reintervention or extraction
“The resilient nature of bacteria, combined with often complex root canal structures, make disinfection challenging, leading to a considerable number of persistent infections,” explains Professor Francesco Mannocci, one of the study’s authors and a professor of endodontics at the Dental Institute at King’s College London. “This is one of the main causes of root canal treatment failures.”
More emerging research: Could this drug meant the end of dental fillings?
Created by Mannooci and group of fellow researchers at King’s College London, SafeRoot detects residual live bacteria in the root canal area using Calcein acetoxymethyl, a florescent dye, and fluorescence microscopy/spectroscopy. In clinical trials, the process, which is performed during the root canal treatment and uses standard sterile endodontic paper points for sampling, successfully detected bacteria after three minutes of testing.
Professor Tim Watson of the Dental Institute believes that the short amount of time the testing takes is a huge benefit. “SafeRoot will reduce the time for root canal completion and will increase the success rate of treatments by letting the dentist know when it’s safe to proceed with filling the tooth,” he says. “This should produce fewer acute ‘flair-ups’ and failed root treatments, as any residual infection in the root canal will be identified.”
With over one million root canal treatments conducted in England every year, preventing the need for secondary appointments could save the National Health Service, England’s publicly funded national healthcare system, a significant amount of money. The monetary savings would be substantial in the United States as well: According to the American Association of Endodontists, more than 15 million root canals are performed every year in the US.
“The treatments are not only time consuming and painful for the patients, but cost … a significant amount,” summarized lead researcher Dr. Frederic Festy. “If we could reduce the number of root canal treatments and re-treatments required, it could mean sizeable savings.”
But as Dr. Festy mentioned, money isn’t the only issue: reducing the risk of secondary infections could make procedures less painful-an attractive incentive to patients, 67 percent of which say pain is their biggest fear when it comes to root canals.
Trending article: How to simplify endodontics with technology
In addition to root canals, SafeRoot could also be used for infection detection in other medical situations, such as wound treatment or implant-related infections. “This technique could be applied to antimicrobial research and disinfection control in clinical settings,” the study reports.
Other research from UCLA published in the journal ACS Nano also explored how to eliminate the risk of secondary infection, using gutta percha infused with nanodiamonds. Nanodiamonds, tiny particles formed as byproducts of diamond refining and mining, are thousands of times smaller than the width of a human hair. They have been widely explored for use in dentistry, imaging and regenerative medicine, among other uses.
The nanodiamonds were loaded with amoxicillin, a broad-spectrum antibiotic, and infused into the gutta percha. Although the nanodiamond-infused gutta percha did leave small gaps in the canal, it was found to fill the space as effectively as the traditional formula-with the added bonus of effectively preventing bacteria growth.
The full SafeRoot study, “Rapid bacterial detection during endodontic treatment,” was published in the Journal of Dental Research.