“You’re Looking At a Material that’s Reasonably Bulletproof”
Researcher and clinician Ken Malament, DDS, explains the conclusions reached by his 16 years of longitudinal research using Ivoclar Vivadent’s IPS e.max Press material.
In a very simplified sense, restorative dentistry comes down to removing diseased or decayed material and replacing it with something designed to replicate its shape, shade, and strength.
The choice of material for filling the negative space created by the preparation is informed by numerous factors, including the tooth being restored and the patient’s age and various demographics. At the most basic level, the material chosen must be capable of adequately replicating the restored tooth’s function while protecting from further decay and not causing harm to other teeth in the patient’s mouth.
Of course, form is a consideration almost as important as function, and the esthetics potential of the material is another choice. This drive for more natural-looking materials has led the industry to move away from gold and other precious metals for indirect restorations, and away from amalgam for direct restorations. But this shift toward tooth-colored ceramic and composite materials has not been without some trade-offs. Most newer dental materials do not provide the same durability and longevity as their less esthetic predecessors.
Studies continue regarding the wide range of dental materials constantly being introduced. However, Ken Malament, DDS—researcher, practicing dentist, and clinical professor at Tufts University School of Dental Medicine—believes the ideal answer, already widely used, is Ivoclar Vivadent’s IPS e.max lithium disilicate material. He also believes he has the data to support his belief, in the form of 3 studies showing e.max restoration survival rates during periods of 10, 10.9, and 16.9 years.1-3 Dr Malament says he hopes his research helps people understand the benefits of this established material option.
“I hope that people can finally get an understanding that e.max is generally bulletproof,” he says. “If I had to put something in my own mouth, or if I had to put something in my wife’s mouth or anyone’s mouth, I would want a material that is going to last a long time.”
Research Reports
IPS e.max is a lithium disilicate material classified as a glass ceramic. It has been a popular restoration option because of its high strength, high translucency, ideal esthetics, and durability. It can be produced via either the lost-wax pressing technique or via CAD/CAM milling, with the resulting restorations exhibiting similar physical characteristics. The material can be chemically bonded in place, which Dr Malament says is a key benefit.
First introduced to the dental industry in 2004, the material offers the strength for use in posterior restorations that must be able to withstand strong bite forces, but also the esthetics for use in the anterior region. IPS e.max also provides clinicians with a minimally invasive indirect material object because it can be used to create veneers as thin as 0.3 mm, and crowns with walls as thin as 1.0 mm.
Dr Ken Malament’s database includes close to 40 years of data tracking performance of materials used in more than 8000 restorations. – Image courtesy of Ken Malament, DDS
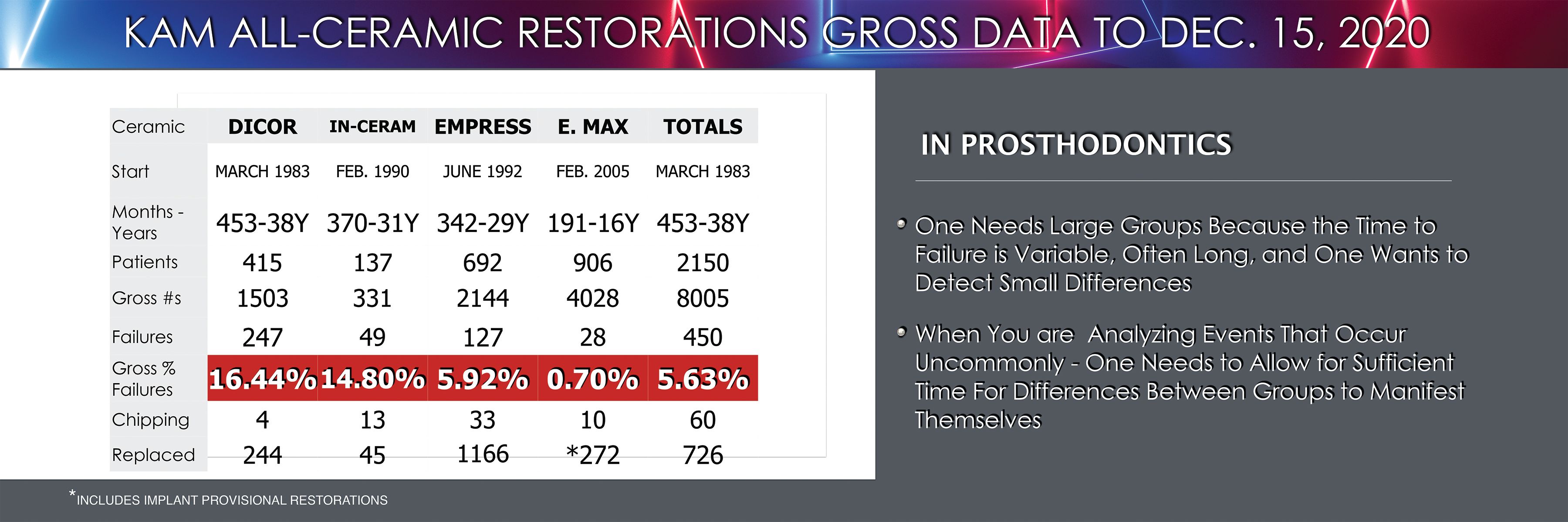
Dr Malament’s IPS e.max research is built on a restoration database he has maintained since 1982. The database tracks the materials used, the type of restoration placed and where it is placed, patient demographics, and whether the restoration failed or was removed for any reason, among other metrics. This allows him to look back on the details of more than 4000 IPS e.max restorations he has placed.
The data he has collected show the durability and generally long service life of the IPS e.max restorations he has placed. He says that during the more than 16 years he has used the material, his database has logged just 28 true failures, even though some other restorations were removed and replaced for other clinical and cosmetic reasons. Consequently, IPS e.max is his go-to option for minimally invasive and partial coverage restorative cases. In the past he would have done these restorations in gold, which has served in some patients’ mouths for more than 50 years, but even though he is not certain a ceramic material will ever last that long as a dental restoration, IPS e.max has certainly proved its worth as an esthetically better, lower-cost option than something cast in gold.
“This is the minimally invasive dentistry. This is partial coverage dentistry. And in the past, partial coverage in my world, and my generation, was all gold,” he says.
Longevity and Versatility
With his decades-long track record of dental material research, Dr Malament says IPS e.max has proved to be the most reliable material he has ever used or tested. His 16.9-year study found a failure rate of just 0.7%, which is far better than other materials he has studied, including zirconia.
Even more telling, his 3 recent studies all found no statistically significant difference between different types of restorations fabricated from e.max. Similarly, the restorations showed no difference in performance when evaluating where in the mouth the restorations were placed, nor any demographic differences between patients. Even the thickness of the restorations did not greatly affect whether a restoration would fail.
“When you go to look at the 17 years [of research], there is no statistical significance between patient age or any other factor whatsoever, which means you’re looking at a material that’s reasonably bulletproof. And we’ve never had a material like that before, except gold. But gold has other problems,” he says, noting gold doesn’t provide the esthetics patients want these days, it also is potentially more temperature sensitive, and bacterial plaque sticks to it far more than a smooth ceramic.
The 10.9-year study of partial coverage monolithic IPS e.max restorations reports an estimated cumulative survival rate of 95.6%.2 The 10-year estimated cumulative survival rate of full-coverage crowns was even better at 99.6%.3 In the 16.9-year study of full and partial coverage crowns, Dr Malament reports an estimated cumulative survival rate of 96.49%.1 All of this points to IPS e.max as a material capable of providing patients with a long-term solution.
Dr Malament notes that he does a lot of partial coverage restorations using different materials, and he remains impressed at how rarely IPS e.max restorations break. He is now researching ceramic failures to gain a better understanding of how different ceramic dental materials break. One trend he is starting to see is that failures with IPS e.max partial coverage restorations are often related to a flaw in the prep design, which can then apply bending forces to the material.
“I would say that the failures that I’ve had—the few that I’ve had—generally are related to me, where I perhaps didn’t prepare the box to the isthmus deep enough. That could create a bending moment. But you clearly see that the survival rate at 98.3% is really extraordinary for onlays. And overall, a 96% survival rate [for both inlays and onlays] over 10 years is extraordinary,” he says.
Forming the Best Bond

This reconstruction for a patient with anterior bruxing involved multiple crowns following periodontal treatment. These IPS e.max crowns still look great at an 8-year recall appointment. – Images Courtesy of Ken Malament, DDS

Another key factor powering the success of IPS e.max restorations is the material’s affinity for creating a strong bond to dentin and enamel when etched, Dr Malament observes. Etching has been an important part of his bonding protocol going back to his use of dentistry’s earliest castable glass ceramic, Dentsply’s Dicor.
“I’ve been studying statistics with dental restorations for almost 30 years, and we’ve never worked with anything even close to [IPS e.max], and I think part of it is because you can etch it and bond it,” he says.
The technique used to secure the material into the patient’s mouth could be considered an extension of the material itself, and Dr Malament also finds the material generally provides a good fit and a tight marginal seal. Lithium disilicate is also easy to identify in radiographs, making margins easy to observe.
“I almost can’t remember any e.max restorations that decayed underneath the ceramic itself,” he says.
This is important because these bonded restorations are demonstrating they are not likely to debond and fall out, which Dr Malament says is something he frequently hears about from friends placing cemented zirconia restorations. Given the track record of success, Dr Malament says using another material when lithium disilicate could be used isn’t logical.
Fabrication Factors
While all 3 of his recent studies examined restorations produced with the press technique, Dr Malament also places milled lithium disilicate restorations, and he has data showing they are just as reliable. The final material being placed in the mouth is the same lithium disilicate whether it was milled and fired in a furnace or pressed using the lost-wax technique. In fact, he believes IPS e.max would be used even more widely and for a larger range of restorative situations if it were available in the puck format used in many dental lab mills.
So, although Dr Malament has placed thousands of IPS e.max restorations, the reason the majority are pressed is that he enjoys working with expert lab technicians in his practice, and he’s been able to work with some of the best in the world.
“I really feel that dental technology is still—even with CAD/CAM and everything else—the heart and soul of the dental industry,” he says.
Although he enjoys collaborating with technicians, one of the things he likes about the material is that it doesn’t always require a master technician’s hand to achieve lifelike lithium disilicate restorations. This is because the material can easily be cut back in key areas and layered back up to add shading and translucencies.
Dr Malament says IPS e.max is the easiest material he has ever worked with when it comes to achieving the desired shade. He sees the material as a great choice, whether it is being sent to a lab for press fabrication and finishing by an expert technician or being milled and fired with some esthetic details added chairside for a same-day appointment.
“Great dentistry is about the materials applied more than the technology used,” Dr Malament says.
Location, Location, Location
Not only has Dr Malament’s research demonstrated the longevity of IPS e.max, but it has also validated the material’s versatility. All 3 of the studies found no statistically significant differences in the performance of restorations based on where they were placed in the mouth. In his experience anterior restorations have almost never failed, and there is always a greater risk of failure for restorations in posterior teeth.
“When you look at the posterior where people would say, ‘Oh no, you must do zirconia here,’ I don’t believe that at all. Not at all. IPS e.max is generally and reasonably bulletproof,” he says.
His research points to IPS e.max as an ideal choice for any inlay or onlay, and also as an equally sound choice for full coverage crowns in all areas of the mouth. It has the strength needed to function in the posterior, has been shown to be kind to opposing dentition, and as Dr Malament’s research shows, provides long-term form and function for patients regardless of where it is placed, who the patient is, or whether it is used for full or partial coverage. He believes his data demonstrate that lithium disilicate is an ideal material for many indirect restorative situations.
“It’s really our choices that ultimately tell us what the patient experience will be like. In the end, it’s the decisions that you make,” he says.
References
- Malament KA, Margvelashvili-Malament M, Natto ZS, Thompson V, Rekow D, Att W. Comparison of 16.9-year survival of pressed acid etched e.max lithium disilicate glass ceramic complete and partial coverage restorations in posterior teeth: performance and outcomes as a function of tooth position, age, sex, and thickness of ceramic material. J Prosthet Dent. Published online September 30, 2020. doi:10.1016/j.prosdent.2020.08.013
- Malament KA, Margvelashvili-Malament M, Natto ZS, Thompson V, Rekow D, Att W. 10.9-year survival of pressed acid etched monolithic e.max lithium disilicate glass-ceramic partial coverage restorations: performance and outcomes as a function of tooth position, age, sex, and the type of partial coverage restoration (inlay or onlay). J Prosthet Dent. Published online October 1, 2020. doi:10.1016/j.prosdent.2020.07.015
- Malament KA, Natto ZS, Thompson V, Rekow D, Eckert S, Weber HP. Ten-year survival of pressed, acid-etched e.max lithium disilicate monolithic and bilayered complete-coverage restorations: performance and outcomes as a function of tooth position and age. J Prosthet Dent. 2019;121(5):782-790. doi:10.1016/j.prosdent.2018.11.024
