8 dental implant tips you need to know
It's no secret that implants are here to stay - but are you getting as much out of them as you can?
Dental implants first appeared in the 1980s, but they were expensive and required specialists who could both make and place them.
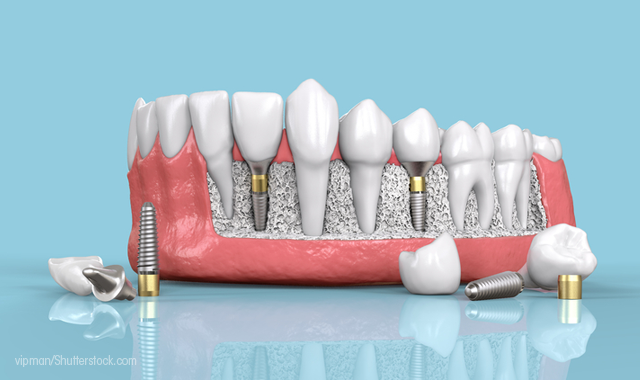
But, like any technology, implants have evolved to the point where they are now very common and can be placed by general dentists. As such, they should definitely be a part of your lab’s products.
Related article: 5 ways technology has changed the implant workflow
There's a lot more to implants than just offering them - technologies and technologies from even just a few years ago just won't cut it in the competitive market. If you're going to offer the best services to your clients, then you need to have the right tools and know-how to stay ahead.
Whether yours is a lab brand-new to dental implants or a seasoned implant veteran, here are a few things that you should know.


It’s good for business
One of the most important things to know about dental implants is what they mean to dental labs, from a business perspective. Labs embracing implants are realizing fantastic success and growth.
“Implants are booming,” Steve Tapie, implant manager at Keating Dental Arts observes. “It’s becoming one of our top products in the laboratory. It seems to just be taking off.”
Tapie says that in addition to the regular marketing efforts (including advertising to doctors, dental societies, at trade shows and on social media), patients themselves are asking for implants. Ultimately, implants tend to be the ideal restorative.
“The patients out there and the doctors are placing more implants restoratively, and for the health all the patient, it is a better restoration,” Tapie says. “Back in the day, you would replace one tooth and do a three-unit bridge. Now, you can replace one tooth and not damage the adjacent teeth. I think it’s becoming more and more common for the doctors to place implants. They’re getting a lot more comfortable. A lot of the general practitioners are placing implants, rather than going directly to a surgeon.”



Compatibility
Implant components can come from different manufacturers. And whether or not the components will successfully work together depends on whether or not they have been effectively compatibility tested.
“Compatible has many different definitions,” Mark Ferguson, general manager at Vulcan Custom Dental says. “When we test for compatibility, it is far more extensive than I’ve seen out of traditional dental labs. When we test for compatibility, it requires quite an investment in parts so you can really understand tolerances and do fatigue testing, and things like that. It’s not just, ‘Measure a few things and see if it fits.’ There’s a lot more to it when you really break it down.”
Compatibility, he says, requires some initiative on the lab’s part.
“They should be asking the question of what type of compatibility testing people are doing,” Ferguson says. “Are there fatigue tests? For instance, when you're looking at a compatible custom abutment. Sure, it might fit, but are companies doing fatigue testing on the implants for those other systems to make sure that while their part may seem to fit, is it going to prematurely wear a different company’s implant? It’s more just an issue of asking what the company’s testing was when they say ‘compatible.’”



Screw-retained restorations
While cement-retained implants are the most prevalent style of implant, Jason Atwood, CDT, senior digital solutions advisor, Core3dcentres, says screw-retained restorations have their place, especially with unique design considerations.
“With a screw-retained restoration, it’s going to be mostly a hybrid-style restoration that will have a full-contour, monolithic-type or ceramic-type restoration, usually zirconia,” he says. “But some people have ventured into other types of ceramics, like lithium disilicate, and there are some considerations there. If you’re opting for esthetics, some people will try to go for the lithium disilicate, but the strength of it is an issue, and I don’t recommend it for certain applications. If the conditions are right, of course, it is usable.
"But an alternative that is really catching on and is doing well is to do a zirconia substructure, then just a small cutback, and then stack some traditional porcelain on there for esthetics. We’ve had great success with that. It gives you the strength of zirconia with slightly better esthetics.”
Related article: Cementable, screw-retained or screw-mentable?
The solution is especially attractive, Atwood says, if strength is a factor.
“That is something we offer, especially if it is a large restoration or any kind of situation where we know that it’s going to have a lot of bite force on it and we want to make it as strong as possible,” he says.



Digital dentistry
Labs were the first to embrace digital dentistry, realizing the benefits of CAD/CAM. But for the workflow to be truly all-digital - and to achieve the resulting benefits - the process must start with the doctor. Happily, however, Tapie says that more clinicians are submitting cases digitally.
“It is a trend, but I think it is a trend that is going to keep on going,” he says. “When we get the file in, we order models, we place the analogs, order the abutments and off it goes. The remake percentage on these is a very, very low. There are fewer variables when you do it digitally, because the doctor will scan, and then send that scan to us, and it’s pretty much done. We are cutting out the variables like the transfer assembly not being seated correctly, impression material not capturing the transfer assembly, so there are a lot of different variables being eliminated by not using an impression. We are having a great success rate with it.”
As with any technology, CAD/CAM is always evolving, and that requires labs to be proactive.
Related article: Our 6 Favorite Digital Techniques
“With all the new systems that are out there, with the digital models and the digital models with impression analogs placed in them, that’s also becoming quite a large department,” Tapie says. “We are getting scans from doctors for iTero or TRIOS or 3M scans and models, and then we get the file from the doctor, we can print the models out, design the abutment and then everything shows up at our door in three days, getting the case into production. That is a really quick turnaround time. And that’s actually becoming a lot more common. We have seen it grow from a few a week to several a day.”
Tapie underscores the necessity of labs keeping up on the ever-changing field.
“Keep up with the software,” he advises. “We try to utilize the main brands, be it the Nobel design titanium abutments, or the Zimmer titanium abutments, or the Straumann titanium abutments. Keeping up with the software and the licensing for that is a task, but it keeps us on the cutting edge.


Design details
Getting the best out of one’s CAD efforts requires a knowledge of anatomy, experience, and the capabilities of the design software. There are many subtleties within CAD softwares that technicians may not even be aware of.
For instance, Atwood mentions a feature offered by many manufacturers called a “split style.”
“It’s where you design the abutment and the crown and everything all at the same time, and then when they generate the files at the end, it splits it into two separate files: one for the abutment and one for the crown,” he says. “You’re able to fabricate both at the same time. If you are using outside milling, you’re able to send one file to the place that mills your titanium and another file to the place that mills your crown. It gives you a little bit of versatility, but it also saves you a lot of time in the design, to be able to design the whole thing at once. The split file is definitely a skill that every lab should learn. It’s very helpful.”
The main benefit, he says, is time savings, but it also allows the lab to offer a complete design.
Related article: Technology seems scary - but better results are worth it
“It’s definitely a time-saver, but it allows you to design the substructure so that it fully supports the crown,” Atwood says. “The traditional way of doing it is first you design the abutment and then fabricate the abutment, and then you fit it to the model, and then you do your crown over the top. And that’s fine, if you are consistent. But if you’re using a split file, you can design your crown first, and then tell it to do, say, a millimeter thickness on the crown, and it will design your abutment accordingly, to fit inside the space you want and give you your crown with a uniform thickness, which gives it its strength.”
But split files aren’t the only benefit of understanding your software. The libraries that you use also have their own features - And if you’re not aware of those features, you may be missing out.
“There are a lot of CAD/CAM tricks and tips involved in different libraries that people don’t really know about,” Ferguson observes. “For example, we have a hybrid titanium base for screw-retained, full-arch. In our library, you can cut it off at five different times. We’ve had a number of technicians come by and say, ‘This would be a great feature if anyone could ever implement it.’ And we have generally said, ‘Yeah, we’ve had that for three years.’”
Finding those features is as simple as asking the software developers.
“Ask the people who create the libraries if there is anything unique about their library, like rotating a titanium base; having different cut-off heights,” Ferguson says. “It’s going to be what the developer has put it into their libraries. And it will change, depending on which CAD system the technician is using, as well.”



Materials matter
Just as design and manufacturing systems are evolving, so too are the materials. They are becoming easier to work with, more durable, and more esthetic. Additionally, prices are coming down, giving clinicians more options at more affordable prices.
“There are so many different options that we have out there,” Tapie says. “We can do our traditional titanium abutments through a CAD/CAM design, through the big four systems - Nobel, Atlantis, Straumann, Zimmer - but the materials are also changing, too. It’s gotten to the point where we can use the titanium bases and save a considerable amount of money. For instance, if you want to use a Bruxer crown, they can cost in the high $400s, but if you want to use different materials and different options, you can get that down to almost $300, which is a price range that we have. It just depends on what type of material you want to use. They’re all great materials.”
Examining each case ensures that doctors and patients get exactly what they want, at the best possible price. The result is a better outcome for the patient, the doctor and the lab.
“We usually analyze the case and we get back to the doctor and let them know, ‘Hey, we can save you some money,’” Tapie says. “There are options out there to save money and have it be beneficial for the patient.”
Communication between the lab and the clinician is critical.
“Nobody wants to see a remake,” Tapie says. “If we see something that may potentially have an issue and be a remake, we always communicate. And that’s key. In the implant world, communication with the GP is of highest concern. We have to have communication so they know what they’re going to get. We have to give them something that we think is good for us and good for them. That’s how we grow our business - it’s having good communication with the doctor and having a successful outcome.”



Working with doctors
The restorative team is just that: a team. For the best results, doctors and labs must know what the other is doing. For instance, the lab and the doctor should be on the same page when it comes to scan bodies.
“Have an open dialogue with your doctors about which scan bodies are easy for the lab to use,” Ferguson says. “Doctors are scanning with scan bodies and sending it to the lab, and the lab has to track down where they got the scan body, what library it’s tied to, and things like that. And I think labs should be a little bit more proactive. If they know that their doctors are getting intraoral scanners, they should steer them toward, ‘You should get these scan bodies’ or ‘stay away from these.’”
And, as labs have been in the CAD/CAM workflow longer than most doctors, some instances in which they should take the lead.
“Labs generally know more about scan bodies than doctors, because they’ve been using them in their lab scanners for ages,” Ferguson says. “It’s pretty new to the doctors, and they don’t necessarily understand how a scan body affects the workflow downstream. Trying to be a little more proactive, on the labs side, is really helpful.”



Surgical guides
Atwood also says that labs should embrace surgical guides. These devices fit over the patient’s gums, and allow the implant doctor to know at which location, angle and depth to drill.
“You can do the implant planning with the final restoration in mind,” Atwood says. “It allows a great deal of control as to the placement of the implant. When you use digital surgical guides, you can place the implants, keeping in mind where the screw channel is going to be, how close to the adjacent teeth you’re going to be, the bite forces on the axis of the implant.
"You can really get into a lot of detail, because you’re able to visualize the final restoration, not just when you’re planning the crown or when you’re planning the abutment, but when you’re planning the placement of the implant. It gives the doctor control over a lot more than just the traditional style all free-handing an implant, doing probing and measurements. It’s just a lot more accurate and gives you the opportunity to control the entire process before you even begin the surgery.”
Offering surgical guides can be an additional source of revenue, but Atwood says there is more to it than that.
“It’s an added feature, but it’s not really about making extra money,” he says. “It’s more about having the restorative drive the implant planning. It gives a more complete solution. If you do the digital implant planning, you can actually share with the patient where their implant is going to look in their x-ray before you place the implant. They are better informed. It gives you a chance to plan the final restoration before you even place the implant.”
