The state of dental implants in 2017
Our annual look at innovations in the implant workflow. Over half of the 500,000 dental implants placed in the U.S. every year are placed by general dentists-and that number is growing, according to the American Academy of Implant Dentistry. Thanks to the digital workflow, specifically CAD/CAM technology, more general dentists are gaining the tools and confidence needed to offer implants to their patients.
Over half of the 500,000 dental implants placed in the U.S. every year are placed by general dentists-and that number is growing, according to the American Academy of Implant Dentistry. Thanks to the digital workflow, specifically CAD/CAM technology, more general dentists are gaining the tools and confidence needed to offer implants to their patients.
Technology
“There are many dental professionals who, understandably, are wary of new ways of working and prefer to continue using the processes they were originally trained in,” says Dr. Pascal Kunz, vice president of product management for digital dentistry at Nobel Biocare. “The number of early adopters in dentistry remains relatively small, but those that embrace emerging technologies stand to benefit.”
Technology should help dentists become better, not force them to leave their traditional education and skills untapped. “We have to create even better synergies within the treatment teams,” he says. “I think overall
the industry leaders have realized that digital dentistry has arrived and are beginning to embrace the change that is happening.”
Trending article: What digital dentistry means for implants
How CAD software is impacting the implant workflow
Computer-aided design and milling have revolutionized the implant workflow, according to David Rice, DDS.
“Our ability to diagnostically work up a patient where we can digitally create the final restoration prior to any surgical procedure is amazing,” he says. “We can design and then mill or 3D-print surgical guides, which will give us the exact location for where that implant should go before we begin. When we get to the healed portion and actual placement of the restorative phase, we already know that our final restoration will be in a perfect position, safe from the vasculature and any nerve issues and built for a perfect occlusion and perfect esthetics.” This kind of technology also ensures that labs get more accurate information in regards to timing and relative location of the implant to adjacent teeth. “The laboratory doesn’t have to worry about taking the impression post, manually inserting an analog into it, and putting it back into the impression to then fabricate a custom abutment and crown for the patient,” says Paresh Patel, DDS. “Everything will just be totally in the digital world and not have to go into a tabletop laboratory scanner to then turn it into something that the doctor can give to the patient.”
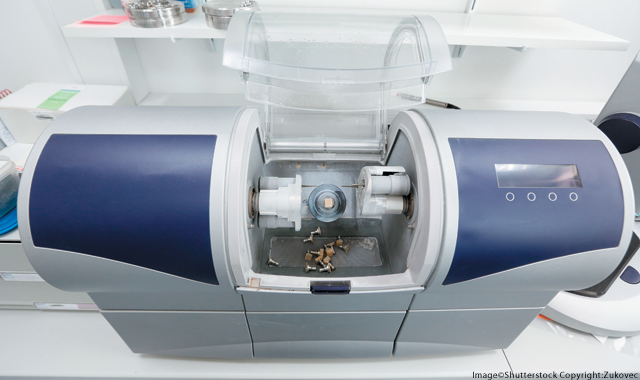
That ensures a more accurate and streamlined process, increasing communication between members of the treatment team and creating a better patient experience, says Priya Menon, director of marketing, North America at Dentsply Sirona Implants. “It’s also a key contributor to the rapidly growing trend of integrating a more flexible and complete digital workflow,” she says.
“We have certainly seen a very strong uptake of Nobel Biocare digital solutions for dental implant treatment,” Dr. Kunz says. “We are seeing significantly more software installations and more cases planned digitally. The option for guided pilot drilling only has also proved popular, with clinicians understanding the importance of achieving the desired position, depth and angulation of the first drill, but then appreciating the flexibility of a freehand approach.
“The importance of fully understanding the clinical situation, including prosthetic requirements prior to treatment, is greatly valued by clinicians. [...] It’s about looking at the bigger picture to help ensure the best possible approach to treatment.”
Trending article: 5 surprising ways digital tools can boost your abilities
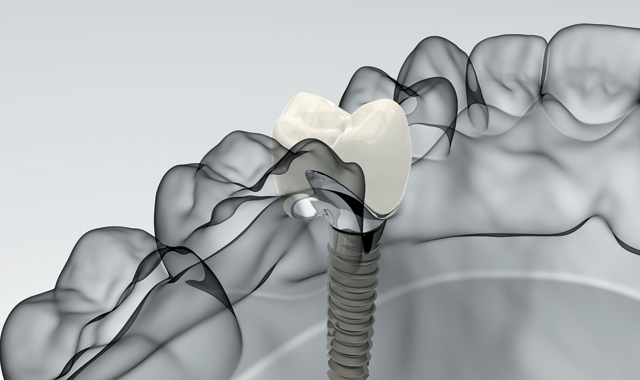
The role of CAD/CAM in implant dentistry also plays a huge role in creating custom abutments.
“We are able to create a custom abutment, just like we used to with a laboratory, and send it,” Dr. Rice says. “Except now, we have total control chairside to design or move a margin on a custom abutment. The number-one reason implants fail today is because dentists are leaving cement. The custom abutment is so impressive because not only can we esthetically design how we’d like our implant placed and positioned, but we can move the finish line where a crown and that custom abutment will interface. That process is super simple. Between zirconia and e.max, we have two very durable and highly esthetic materials to mill our custom abutments out of, from a CAD perspective.”
Dentists also have the benefit of printing surgical guides.
“Using the 3D imaging data, digital treatment planning software enables the clinician to virtually plan their implant case prior to surgery, taking into account vital anatomical structures, bone quality and prosthetic requirements,” Menon says. “From the plan, surgical guides can be produced that allow for the exact replication of the plan to be carried out during surgery.”
According to an October 2012 literature review in the Journal of Oral Implantology (“Types of Implant Surgical Guides in Dentistry: A Review,” by Kathleen Manuela D’Souza, Meena Ajay Aras) implant software cannot override human error, so it is imperative that dentists have the education to understand what goes into placing a long-lasting, esthetic restoration.
“The various complications recorded were related to inaccurate planning, radiographic stent error, intrinsic errors during scanning, software planning, the rapid prototyping of the guide stent, and the transfer of information for the prosthetics,” the authors write. “However, if the clinician recognizes these sources of inaccuracy, efforts can be made to minimize the error and optimize patient treatment.”
Still, companies continue trying to compensate for human error.
“Dentsply Sirona Implants’ VAD (Virtual Atlantis Design) software takes the specific edentulous space, surrounding teeth and soft tissue anatomy into consideration, providing prosthetic solutions that mimic true natural tooth function and appearance,” Menon says. “Engineering principles are built into the software to ensure the requirements for manufacturing precision and integrity of the design are maintained, thus eliminating the errors that can occur with human designs using computers.”
Patients are getting in and out of the chair faster
Another result is time saved. “Once the clinician has the information of a patient’s dental anatomy captured digitally, they can perform all the treatment planning in a virtual environment,” Menon says. “Having this information and plan allows the implant procedure to be executed with precision with surgical guides, and even allows for a temporary restoration to be designed, manufactured and available on the day of surgery.”
“If you did a direct comparison of chair time, it may be the same,” Dr. Rice says. “But it’s much more efficient for patients. Sometimes a patient will stay for a longer appointment and sometimes they’ll choose to come back for a second appointment, just like they have in the past.”
Trending article: Changing the future of implant dentistry with robotics

How technology has changed the placement procedure and the ability of doctors to ensure implant success
Dentists benefit from technology from the very first step, Dr. Patel says.
“We can start straight from diagnosis and treatment planning,” he says. “With technology bringing the cost of cone beam down, I really don’t see anyone wanting to buy digital panoramas anymore just because the volume of information that we can get with a CBCT scan is so much greater (with an equal or maybe even lower radiation dose in certain cases) as well as the ability to focus on a specific area we want in an image of a 3D scan.”
Dr. Patel can plan a surgery that he feels confident performing. He can also refer the case out if it requires additional bone or soft-tissue grafting or bone expansion.
“We can plan the appropriate-size implant, the trajectory, the depth of it and the timing of the implant,” he says. “We can go ahead and have the laboratory create the surgical guide. If we wanted to, we could even have the laboratory create a screw-retained temporary for our patient and plan out the occlusion of the opposing arch.”
All of these options, he says, would be very difficult without a cone beam. For other doctors, a 3D printer is a welcome addition to their arsenal.
Trending article: New discovery could reduce the dental implant failure rate
“I think a lot of doctors are now taking advantage of [3D printers] to plan their cases,” Dr. Patel says. “They can send it to a 3D printer in their office and within a few hours have a surgical guide that they can sterilize and put in their patient’s mouth to place the implant with confidence-placing it where they want it to be placed, avoiding vital structures and having the trajectory that they want.”
Another major benefit of the digital workflow, of course, is greater communication between the dentist and laboratory. That means fewer mistakes from the beginning: Problems are being anticipated before they have to be corrected.
“In traditional workflows, clinicians and labs were quite disconnected,” Dr. Kunz says. “The lab technician was far too often confronted with implant positions that did not adequately take prosthetic requirements into consideration. The lab tools available were largely aimed at ‘bailing out’ such less-than-ideal implant placement instead of preventing mistakes on the clinician’s side in the first place.
“The latest digital solutions have evolved to become more adaptable, offering greater involvement of the dental technician before decisions on final implant positions are made,” he continues. “The needs of every patient are unique, and today’s workflows are becoming as varied as their needs.”
One aspect of improved creation is the influx of open files so that both sides can integrate new solutions into equipment they already own, he says.
“Developments in IT hardware have played an important role too, of course, from graphics cards that allow faster, higher quality visualization to networks and equipment for greater connectivity. [...] Such developments allow improved collaboration that benefits both the treatment team and the patient,” he says.
How imaging ensures better and more assured results
Greater imaging capabilities also facilitate better patient education and, therefore, case acceptance.
“The advantage is having optical imaging and cone beam imaging that we can combine together, not only to make the surgical and diagnostic phase easier, but really as a benefit for the patient,” Dr. Patel says. “It makes selling the case easier because the patient can understand what they’re looking at and can see what we have to deal with. If we can’t do the case, the patient understands why.”
Patients also have the benefit of seeing that their dentist has a solid understanding of the physiology of their jaw and teeth and can feel more confident in the treatment plan.
“Digital imaging obtained through the use of a CBCT scanner ensures a highly accurate 3D image of anatomical structures and information about the patient bone quality and architecture, providing insight and confidence of accurate implant treatment planning,” Menon says. “When the CBCT and intraoral scan are brought together for case planning, the position of the implant can then be based on a restoratively driven, crown-down approach for optimal function and esthetics.”
Trending article: The future of implants is here
How technology has improved the practical aspects of implant work
“For me, the most impressive part is the ability to treatment plan,” Dr. Rice says. “I think most dentists underestimate that that is the pivotal step of this process. If you plan it well in the beginning, the rest of the workflow just cascades.”
Dr. Rice appreciates that he can use cone beam and CAD/CAM to determine if an implant can be placed within 15 minutes. That’s a huge change from the previous workflow.
“On the spot, you already know what a patient needs to do in order to place that implant or what you need to do if you can’t, as opposed to making impressions and all this other stuff and two weeks later figuring it out.”
Trending article: 5 things hygienists need to know about dental implants
He adds that chairside has brought dental 360 degrees. “Dental implantology started with screw-retained implants,” he says. “We got away from it because we didn’t have the materials to esthetically make that happen, but now with CAD/CAM and e.max and zirconia in monolithic forms, we’ve come full-circle to being super safe and choosing the best restoration for our patient.”
He says that it’s allowed dentists to make an unbiased decision for their patients. “In the beginning, screw-retained was popular because it was the best we had,” he says. “Then custom abutments and crowns came in vogue because everybody was told that was the best that we had. Now, because of the technology, we legitimately have the ability to produce either option. It’s about what restoration makes the most sense for our patient.”
Innovations in implants
For edentulous patients, having an esthetic, functional option for replacing missing teeth is essential.
“There is a crucial need to replace lost teeth that not only resemble natural teeth, but provide the function and comfort of them as well,” Menon says. “With dental implant options that address the whole gamut of tooth replacement, patients are being provided with the most vast, reliable range of therapy options than ever before.”
The market is there, of course, so innovations in the realm of dental implants abound.
“For clinicians to meet increasing patient demand for immediate teeth, they require implant systems with a macro and micro design and drill protocol that enable immediate loading protocols,” says Stefan Holst, DMD, vice president of implant systems and research at Nobel Biocare.
He says that Nobel Biocare’s lines of implant systems have shown success in studies conducted up to 10 years after placement.
“But even such documented long-term performance is not a reason to stop innovating,” he says. “Some suggest there can no longer be significant further innovation in implantology. This is absolutely not the case. There is great potential for further enhancements to products and protocols in order to further reduce time-to-teeth for dental implant patients while at the same time increasing safety and predictability of treatment procedures.”
Trending article: How implant surgery can help both you and your patients

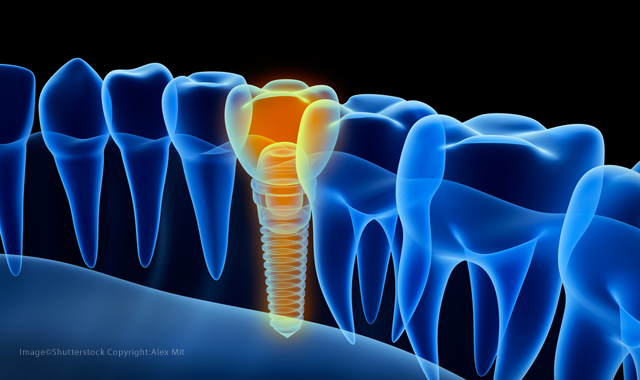
Focus on osseointegration
When it comes to how successful the implant is and how the tissue surrounding it responds, it’s all about the surface of the implant.
“Advancement in implant design, tighter implant-abutment connections and advancements in implant surface technology allow for implant therapy to be more predictable and reliable over the long term by allowing for improved immediate implant stability and faster osseointegration of the implant,” Menon says.
“The surface coatings that are on dental implants today are the key,” Dr. Rice says. “It’s the chemistry behind what the titanium is plated with that makes integration so predictable.”
What he means by surface coating is the use of an SLActive surface, an implant design from Straumann that “takes the scientifically proven SLA surface one step further through its improved surface chemistry.” Because it is a hydrophilic material with a high surface energy, it is able to achieve secondary stability sooner, helping to avoid the stability dip often seen on implants around four weeks after placement.
“Implant surface coating is all about SLA active materials,” he says. “All the best companies utilize it; it’s a major asset for osseointegration.”
Related reading: Implanting success: The state of dental implants
Because today’s implants are not merely machined implants, there is a greater variety in terms of how companies try to improve osseointegration.
“Whether [it’s by applying] an active surface to the implant or it’s by blasting the implant to make you have more surface area, all of that comes with a cost,” Dr. Patel says. Clinicians should be mindful of the risks, he says. “Every time we make the implant surface a little rougher, it increases the potential that we lose some bone support around the implant. How is the tissue going to respond to that?”
Nobel Biocare also utilizes a rough surface on implants, says Dr. Holst. “The role of the implant surface in successful treatment outcomes should not be underestimated,” he says. Their surface, called TiUnite, “is a thickened, moderately rough titanium oxide layer with high crystallinity and a high phosphorus content.”
Again, when it comes to choosing an implant system, it’s not a one-size-fits-all decision. With so many options out there, dentists should ask questions to find out which one is best for them, Dr. Patel says.
“We have to be careful to choose an implant system that is well conceived, the surface area and the surface treatment makes sense, and gives us options for placing that implant. Can we place it with flexibility? Can we place it equicrestal, supracrestal or subcrestal? I like to use an implant system that has a machined collar on it because no piece of bone is going to be 100 percent flat. It gives me the flexibility to place an implant where the bone and tissue will be happy against it.”
How bone regeneration is changing
“On the bone grafting side, the greatest game changer for the general dentist especially is socket preservation,” Dr. Rice says. “Plasma-rich proteins and socket preservation upon extraction are some of the things just setting us up for massive success. We’re not dealing with major bone defects. We’re dealing with healthy bone and a good quantity of it to work with from the beginning.
“When I graduated from dental school, you took a tooth out and then if you were going to have a dental implant after it healed, you might go back in and surgically create a flap graft with bone, let it heal again. In today’s world, we have the ability to preserve the socket upon taking the tooth out. You’re creating a hole where the tooth used to be, you’re filling the hole with products that stimulate our body to regrow its own bone. As long as you have 360 degrees of natural bone around everything in the middle, your body just knows what to do because we can influence it.”
Trending article: How technology is changing the game for dental implants
Dr. Patel believes the landscape has changed drastically over the past five to 10 years.
“We have so many new biologics that have come on board,” he says. “Certainly, mineralized freeze dried bone or demineralized freeze dried bone or combinations of those products are everywhere and are easily accessible. Collagen membranes are accessible. Patient-driven biologics such as PRF are very easy to produce. It’s a great time to get involved in growing bone and tissue so you can place an implant in the most appropriate spot and also to increase your long-term results. Now, we’re finding that we’re doing more thickening of the tissue with something like an alloderm in addition to trying to grow back bone or, if we do an extraction, to preserve bone.”
Menon says that the need for regenerative material hasn’t grown, but tissue regeneration has become more mainstream.

“There is still debate around the effectiveness of these products and a high price tag associated with them, which does not help the matter,” Menon says. “With respect to more established product types like grafting material and membranes, there is higher demand for easy-to-use packaging and products.”
Since product performance is predictable, he says, the biggest criteria involved in selecting a product is convenience in terms of handling, use and hydration.
“Clinicians appreciate more user-friendly packaging of bone grafting granules like a dappen dish or syringe for easy accessibility and use,” Menon says. “On membranes, a newer collagen membrane like the Symbios pre-hydrated membrane offers more convenient handling by packaging it in saline to completely bypass the time-consuming hydration step in the surgical procedure.”
Trending technique: How to place implants quickly and precisely using CBCT
The benefit of all these enhancements is dentists have more options-leading to more price points and greater affordability.
“Now there are so many implant companies out there, you can find the implant company you want to work with, as opposed to choosing from a few players,” Dr. Patel says. “That has put downward pressure on price, so you can buy an implant system that makes sense and an implant that is well-crafted and well-conceived without having to spend thousands of dollars to get involved in implant dentistry or spend several hundreds of dollars to get a quality implant. There are plenty of implants out there that offer that to a general dentist at several price points.”
Though these technologies and materials are making it easier for general dentists to expand into of implant dentistry, it does not circumvent the need for a skilled laboratory technician, Dr. Kunz says.
“While technologies come and go, the human qualities of a skilled, local dental technician remain invaluable,” Dr. Kunz says. “As I see it, the best way for a laboratory to fend off competition from remote providers is to take greater advantage of the personal service they are able to offer. It’s this that can truly form the basis for long-lasting partnerships. Technology should facilitate this relationship, not replace it.
“While options exist for other dental professionals to work on the prosthesis, we still believe that a trained dental technician is best placed to develop high-quality prosthetics,” he adds. “And, when we consider that the implant and the restoration work as one system in the mouth, this is crucial for high-quality treatment outcomes. And above all, it’s in the best interests of the patient.”