How to streamline the cementation of crowns
With the rise of all-ceramic restorations, it’s more important than ever to consider your cements carefully.

Dentists, more than ever before, are able to deliver some absolutely beautiful, lifelike and well-fitting final restorations. The pendulum has swung from the predominantly porcelain-fused-to-metal market to all-ceramic restorations, driven by lithium disilicate and zirconia substrate options that offer esthetics and durability.
Because of these materials’ dominance, it is important to look at the cements chosen for final placement, their composition and mechanisms used by which to secure the final restoration placement. Securing a final indirect restoration has moved well beyond just conventional luting or cementing.
Gone are the days of sole reliance on mechanical retention. Adhesive cements are readily available that provide both chemical and mechanical retention. These cements allow clinicians to rely on specific adhesive features that enhance the bond strength, create an efficient workflow and provide a more confident outcome.
Related article: 4 big benefits of resin cements
The current landscape of cement choices is complex to navigate, and without a strong foundational knowledge of what cementation strategy to implement, cementation failures can occur. Clinical consideration must be given to the retention and resistance form of the preparation, margin placement, preparation of the intaglio surface of the restoration and adhesive cement characteristics, along with possible light curing to facilitate easier marginal and inter-proximal clean up.
Here are some pointers to help dentists and their assistants steer through the decision-making process and determine which cement offers the best potential benefit given the clinical presentation.
Preparation
Begin by assessing the design, height and taper of the tooth preparation because this will determine whether the restoration needs to be cemented or bonded. The purpose of any cement is to fill the micro-gap that exists between the restoration substrate and the tooth. The cement translates the retention form of the preparation to the restoration.
More ideal preparations permit traditional cementing options as well as allow for adhesive protocols. For those preparations that are clinically short or have a taper greater than 20 degrees, those indirect restorations will require bonding or an adhesive protocol.
Cement choices
Understand that modern adhesive resin cements offer versatility in how they are placed and cured. They are usually a one or two paste system, delivered in a syringe and often coined “universal cements” because they allow for the clinician to choose which of the three bonding mechanisms is appropriate given the clinical case.
Related article: How to achieve esthetic results with direct composites
Adhesion occurs via a total-etch method, which requires etching of the tooth accompanied by a bonding agent application; self-etch modality whereby a self-etching adhesive is applied to the tooth preparation prior to cementing; and a self-adhesive method, which is closest to traditional luting in that a bonding agent is not required.
Light curing
Another differential in all of these cements is their curing mechanism - some offer the ability to be light cured, while others require a dual or chemical cure. Keep in mind that light does not pass through zirconia, so when using this particular substrate, you must use a dual- or chemically-cured cement. Additionally, many of these cements feature a “wave or tack” cure of three to five seconds at the margins. Essentially, the tack cure facilitates an easier clean up around the margins while the cement is in a more gel-like phase.
Continue to page 2 to see a case study...
Substrate preparation
Central to the cement’s performance is how well it will integrate with the substrate of the restoration. To achieve optimum bond strength, intaglio surfaces must be properly prepared. Zirconia surfaces require air abrasion of a 30-micron particle size for 10 seconds at 30 psi.
Next, a primer application can follow that is specific for that particular substrate. On the other hand, do NOT air abrade glass ceramics! This may initiate internal cracks or fractures. Instead, apply a 5% hydrofluoric acid to the surface to create a retentive surface. Rinse, then follow with a ceramic primer application that is allowed to air dry.
Other benefits
Evolving with the consumer demands, many cements are offered in several shades for improved esthetics. Another key feature is the specific monomers included in some formulations - MDP and 4-MET(A) - to ensure improved bonding values. Essentially, there is no need for a separate adhesive primer. This greatly reduces the risk of contamination, inventory and any errors that could affect the quality of the bond between the cement and substrate.
Case study
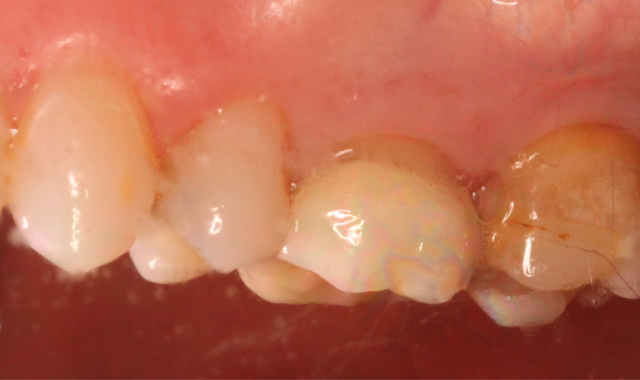

Fig. 1 Fig. 2
A 53-year-old male presented with a treatment plan to replace an existing f rst molar crown and prepare a crown on a second molar (Figs. 1-2).
The patient was anesthetized and tolerated the crown preparations well. Both zirconia-style preparations were digitally scanned and those scanned impressions were sent to an off-site lab. Temporary crowns were fabricated and worn for two days. Upon return, the temporary crowns were immediately removed. Notice the healthy condition of the gingiva (Fig. 3).
At this point, the selection of what cement would work best enters the decision-making process. Taken into consideration is the height of the preparation and taper. Both preps are retentive. This allows the choice of either bonding or traditional cementing.
Given the three classifications of bonding mechanisms earlier mentioned, a self-etching adhesive resin cement, SoloCem® (Coltene), is selected. SoloCem offers a one-step bonding approach to final cementation that reduces the risk of contamination during the process and also includes the MDP and 4-MET(A) monomers that ensure good bond strength to the zirconia substrate - no additional metal primer monomer is needed (Fig. 4).


Fig. 3 Fig. 4
Both preparations were scrubbed with 2% chlorhexidine to remove any residual cement or debris. Both zirconia crowns were scrubbed with Ivoclean® (Ivoclar Vivadent) - a decontaminator - for 20 seconds, then thoroughly rinsed and air dried. A frosty internal surface appeared on both crowns.
Care was taken to directly load the crowns evenly with translucent SoloCem. SoloCem is a two paste system that is delivered in an automix syringe. It offers low shrinkage, high sheer bond strength, low water sorption, increased radiopacity and excellent bond strengths to dentin.
Because the monomers are already added to the cement formulation, the workflow was more efficient and certain of introducing no contamination. This is an important benefit, especially when performing quadrant dentistry (Fig. 5).


Fig. 5 Fig. 6
Both zirconia crowns were fully seated and occlusion was confirmed. A three-second tack cure followed at the buccal and lingual margins. (Fig. 6) Excess cement was removed and the margins were once again light cured for 20 seconds each.
Again, both restorations were secured during this process. Keep in mind that 90 percent of bond strength in most of these cements occurs within the first 10 minutes, so it is critical to make sure when the restoration is seated, it is secured. Disturbing those early bonds could be detrimental. The final view of the restored maxillary molars is shown in Figures 7 and 8.


Fig. 7 Fig. 8
Conclusion
Many clinicians would define a successful crown or indirect restoration as to whether it “stays on,” but it really is much more than that. To simplify this process, clinicians must consider the value of a retentive preparation, plan for an optimal restoration type and thickness, and depend on a cement’s formulation to adequately bond to the tooth and the restoration in an efficient manner. Given all these variables, that is a lot of trust that needs to stand the test of time.