How Much PPE is Enough?
The National Institute for Occupational Safety ad Health's Hierarchy of Controls offers good guidance on how to remove safety hazards from the practice and how to handle hazards should they appear.
©DCStudio/Stock.Adobe.com

When the coronavirus 2019 (COVID-19) pandemic first broke out last spring, practices scrambled to find adequate personal protective equipment (PPE). The Occupational Health and Safety Administration (OSHA) eased some of its PPE requirements to alleviate the burden on the strained supply chain.
However, OSHA still had to strictly enforce its PPE guidelines for the safety of medical professionals and patients across the country. In fact, in September 2020 the administration cited Georgetown Dental, LLC in Georgetown, Massachusetts for violating respiratory protection—with 6 serious and 1 other-than-serious violation.
But even 1 year into the pandemic, PPE problems still persist. How much PPE is needed? Is anything new necessary? What’s in short supply and where can you go to get it?
What Is Needed
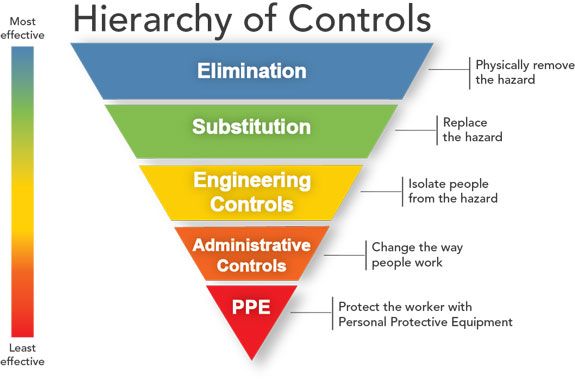
As important as PPE is, it’s easy to forget that it is not meant to be the sole source of protection for dental healthcare personnel (DHCP). The National Institute for Occupational Safety and Health (NIOSH), the research arm of the Centers for Disease Control and Protection (CDC), advises a series of risk mitigation levels, with PPE being the last line of defense. NIOSH’s Hierarchy of Controls are:
- Elimination
- Substitution
- Engineering
- Administrative
- PPE
“Even before COVID, the Hierarchy of Controls is something that you can implement, no matter what the occupational threat,” says Karen Daw, “The OSHA Lady”, speaker and consultant. “It moves you through a series of controls. You would have applied that to bloodborne pathogens. Now, you’d apply it to bloodborne pathogens and COVID, and for the next virus that might make it to us.”
PPE is at the bottom of the Hierarchy of Controls, not because it’s ineffective, but because it’s the least effective safety measure against bloodborne threats, Daw explains, since the Hierarchy was compiled pre-COVID when bloodborne pathogens were a greater focus. Employers should start with a hazard assessment, which is a method of identifying which hazards exist in the workplace, Daw says. Then, the Hierarchy of Controls should be implemented to determine the best method of removing that hazard.
Prior to the COVID-19 pandemic, facemasks, scrub jackets, and eye protection were common elements of PPE, Daw says. But the coronavirus has changed not only the type of protection used, but the quantity practices must have on-hand.
“As far as quantity before the pandemic, it wasn’t uncommon for practices to have a couple of week’s worth in the closet, because it can take up a lot of precious real estate, depending on the size of the practice,” she says.
The New Normal
There’s no doubt that the pandemic has forced the healthcare industry to overhaul its infection control methods. For the dental industry, no infection control issue has been bigger than aerosols. The SARS-CoV-2 virus is transmitted in aerosols, and maybe even lighter, less moist airborne particles, says Jackie Dorst, RDH, BS, an infection prevention consultant and speaker.
“That’s where airborne contamination has become a greater concern for PPE than pre-pandemic patient contact,” she says. “With aerosol/airborne disease transmission, we looked at, how much filtration do we get from the different levels of masks and how can we provide greater protection from those aerosols that are created with aerosol-generating procedures, such as when the doctor uses a high-speed handpiece with water; the dental hygienist uses an ultrasonic scaler with water going through it to cool and to flush the debris away. Water flowing through the device magnifies and increases the number of aerosols that the team could be exposed to during direct patient care.”
A year ago, there was so much unknown about this novel virus and how it is passed person-to-person, how contagious it is, and how to mitigate its transmission. Dental practices and other healthcare facilities had to rely on the CDC’s evolving guidelines.
“Dental professionals have to consider CDC interim guidance during the pandemic,” Dorst says. “And OSHA’s interim guidance during this airborne disease pandemic requires dental professionals to look closely at the different levels of masks. For a surgical, also called a procedural mask, which doesn’t seal tightly around the nose and the mouth, the filtration, and the fluid resistance determines whether if the mask is a level one, a level two, or – the highest level – level three that is going to give the greatest filtration.”
To help determine how much PPE a practice needs, CDC offers its Burn Rate Calculator. It is a spreadsheet-based model that will help healthcare facilities plan and optimize the use of PPE for a response to COVID-19.
Breathing Easy
Because SARS-CoV-2 is spread through aerosols, more focus has been placed on masks and respirators.
“The difference between a mask and a respirator is that the respirator seals completely around the nose and mouth,” Dorst says. “Inhaled and exhaled air must come through the filtering membrane. A procedure mask has gaps around the nose and on the sides where the pleated folds may gap. If you breathe out, air escapes all around that mask. If you breathe in, air enters all around that mask. All air is filtered when wearing an N95 respirator, because of the seal. Air must come through the filtering membrane and, therefore, provides greater protection to the wearer for preventing disease transmission. The big PPE difference, prior to the pandemic, was that very few dental professionals had ever worn an N95 respirator.”
It isn’t as simple as stocking a supply of N95 masks. They must be fit tested to ensure that DHCP is adequately protected.
“When an employee is required to wear an N95 respirator, they must pass a medical evaluation. Medical evaluations can be done online in a confidential manner. It should also be completed before the fittest,” Canham adds. “Passing a medical evaluation and fit testing is mandatory. OSHA requires this before an employee is given an N95 respirator to wear.
The Hierarchy of Controls from NIOSH.
“The common mistake that I see with people who are wearing an N95,” she continues, “is that they’re not performing the seal check each and every time they don their N95 respirators.”
Seal checks aren’t hard to perform, they just necessitate proper training.
“Another OSHA requirement is that employees must be trained properly on the donning, seal check, and doffing protocols. Canham says. “And there are some fabulous 2- and 3-minute videos on YouTube or the CDCs website.”
Fit testing isn’t something that practices need to hire a consultant to perform in-person. One of Canham’s services is a respirator fit testing tool kit for practices. It is available on her website.
“You don’t have to spend, hundreds of dollars on fit testing,” Canham says. “Anybody can do fit testing, as long as they learn how to do it.”
Scarcity
Because of the pandemic, practices may run into shortages. Last year, masks and respirators seemed to be in high demand. This year, gloves are hard to come by.
“For PPE, the supply chain for gowns and masks has been replenished, and those are pretty readily available,” Dorst says. “Respirators in the supply chain was getting refilled. And toward the end of December in 2020, we were seeing that they were still expensive, but they were available. Surgical masks are available. Disposable gowns are available.”
“It’s interesting to see where the shortages occur,” Daw observes. “Initially, it was gowns, and that’s because nobody ever really considered isolation gowns in the dental setting. And now we’re able to find disposable and reusable gowns. That’s not an issue. Then we saw a shortage of disinfecting wipes. Now, people are saying that they’re unable to get their preferred brand of gloves.”
So where can practices turn if they find themselves in short supply of PPE?
“I don’t have a magic cure for that,” Canham says. “I do recommend that dental practices continue to work with their dental supply dealers and document their efforts. Documentation shows the attempt they made to get their PPE, who they called, what date they called, and the result of the call. It is my experience that when OSHA comes knocking, they want to see the documentation of the practice’s effort to obtain PPE.”
In some cases, dental health care workers may have to extend use or use limited reuse strategies for N95s. The CDC website has recommendations on how to do this.
Daw recommends opening accounts with several different companies, reaching out to professional organizations, or even posting on a Facebook Group like her “Dental OSHA and Infection Control” page.
“Sometimes a professional organization can help not only with obtaining, but also distributing PPE. Posting questions related to what you’re experiencing, and then see how other people are managing it, too, will help multiple practices” Daw says. “We’ll get through this. It’s just nice to know that you can turn to your team or even people from all over the country that are part of your tribe. These are the people who you can count on to help you resolve whatever challenges you are facing.”