The foundation of patient well-being starts in the chair
Treating dentomandibular sensorimotor dysfunction boosts profitability and expands the dentist’s role.
Treating dentomandibular sensorimotor dysfunction boosts profitability and expands the dentist’s role.
Dentistry is more sophisticated than it was years ago. New techniques are available for diagnosing and treating a multitude of oral health-related problems, from cavities to edentulism, and from periodontal disease to xerostomia. And, as the association between oral-particularly periodontal-and systemic diseases has become clearer in recent years, so too has the dentist’s importance in helping patients maintain their overall well being.1
Patients and dentists’ physician colleagues are starting to respond accordingly. Today’s savvy and educated patients know dentistry isn’t the “drill it and fill it” profession they once thought it was. Physicians are working with dentists to address a patient’s medical concerns, such as treating and monitoring a patient’s periodontal disease to better manage their diabetes. Additionally, dentists are increasingly among the professionals to whom patients are referred when oral tissues and the temporomandibular joint is the suspected cause of problems. 2,3
The big picture
Such problems not only include pain and popping in the jaw area, but headaches. According to the National Headache Foundation, more than 29 million Americans suffer from migraine headaches, the causes of which include many trigger factors, such as sleep disorders, hormonal variations, dietary factors, and others, that excite brain cells and trigger the trigeminal nerve to release chemicals that irritate and result in swelling of blood vessels on the brain’s surface.
The reaction continues as swollen blood vessels send pain signals to the brainstem, an area that processes pain information.4 Additionally, U.S. News & World Report notes that an estimated 90 percent of the population suffers from headaches, with migraine sufferers losing more than 157 million work and school days each year because of headache pain.5
Although some headache sufferers successfully treat their headaches with over-the-counter medications, nearly 20 percent of Americans with bothersome headaches seek medical attention when these solutions have failed.5 Additionally, non-pharmacological techniques for controlling headaches also are helpful, with these options including physical medicine.4
The dentomandibuar and pain connection
Because the trigeminal nerve is responsible for transmitting pain impulses, as well as the majority of sensations originating from the head and neck region-including dento-facial pain, dentists are well familiar with sites at which these impulses can be altered and even arrested.5 According to the American Dental Association, dentists’ expertise lies not only in treating the teeth and gingival tissues, but also in caring for the muscles of the head, neck and jaw, as well as the nervous system of the head, neck, and other areas.6
During a comprehensive examination, dentists can spot early warning signs in the mouth that may indicate disease and/ or dysfunctional conditions elsewhere in the body.6 Among these dysfunctional conditions are headaches and migraines, tinnitus, poor airway control, sleep disorders, and restricted range of motion and postural adaptations. In addition, dentists may observe symptoms indicating TMJ disorders, clenching with or without torus formation, bruxism, tooth wear, abfractions, tooth fracture/damage, and an unstable dental arch form.
Unifying these conditions and symptoms is dentomandibuar sensorimotor dysfunction, which results from unmanaged and unbalanced muscle forces.7,8 Managing these problems clinically necessitates pain and inflammation control, rehabilitation of the stomatognathic/dentomandibuar system to normal function and range of motion, followed by orthopedic, orthodontic, or restorative stabilization of the oral complex. Unfortunately, until recently dentists have been unable to objectively diagnose these forces or systematically treat and monitor patients experiencing symptoms of muscle and force dysfunction. However, it is now possible for dental practices to incorporate an innovative assessment and treatment technology for managing and monitoring dentomandibuar sensorimotor dysfunction pain through physical rehabilitation of the musculoskeletal physiology.9
A technological approach to patient care
More than 60 years of combined medical and dental experience have been applied to the assessment tools and methods, therapeutic modalities, and hands-on techniques that dentists can now incorporate into their practices. As a result, they can objectively, and in a minimally invasively way, care for patients suffering with the various symptoms of dentomandibuar sensorimotor dysfunction.
Based on years of research involving thousands of patients, TruDenta is a proven assessment and treatment technology that enables dentists to identify and address dental force related problems using equipment and methods approved by the Food and Drug Administration(Fig. 1).
Each assessment and treatment modality in the system is well known and well documented to be effective for its respective use. Technologies and therapeutic approaches used in sports medicine, such as neuroscience and systematic and objective assessment/monitoring, low level laser therapy, therapeutic ultrasound, and microcurrent nerve stimulation, represent the core of the system. This combination of equipment and methods has a demonstrated history of successfully improving and shortening athletes’ recovery from musculoskeletal and force related injuries and are applicable to dentistry.10-15
However, appropriate patient care is predicated on the examination and comprehensive head health, medical, and headache history, as well as a pharmacological assessment, during which the condition(s) that may be amenable to treatment can be diagnosed. The complete system includes a well-described and documented screening and examination process for identifying patients who will be responsive to therapy.
The health histories and physical examination are supplemented by objective findings that include mandibular range of motion (ROM) disability (Fig. 2), cervical range of motion disability (digitally), and TruDentaScan digital force analysis (Fig. 3). The objective examination of forces placed on the masticatory system is significant for determining the extent of the sensorimotor dysfunction, because abnormal, excessive, or imbalanced forces are reliable indicators of dysfunction and injury. These findings are then combined with a standard panoramic radiographic examination, as well as thorough dental, periodontal, airway, orthodontic, and occlusal examinations. The scientifically based and systematic protocol for assessing and treating the dysfunctional dentomandibular sensorimotor condition prior to initiating restorative procedures will enable dentists to comprehensively rehabilitate the patient and relieve their painful symptoms. Then, if restorations are deemed necessary, the most conservative dental procedure that will stabilize the stomatognathic system, regardless of the occlusal philosophy that is followed, can be predictably undertaken following rehabilitation, because the platform for normal function has been established.
The TruDenta system uses specific frequencies, durations, and modulation of therapeutic ultrasound (Fig. 4), transcutaneous electrical stimulation (sub-threshold micro-current), low level laser/light therapy (Fig. 5), and intraoral orthotics, along with other treatment modalities (Figs. 6 and 7), during the rehabilitation process. This combination therapy is proprietary, unique, and proven to deliver consistently lasting pain relief and dental foundation rehabilitation.

Figure 4
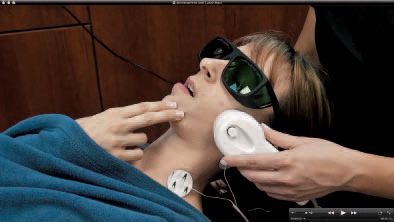
Figure 5

Figure 6
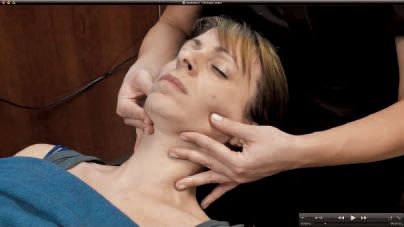
Figure 7
Although dentists perform the assessment stages of patient examinations, treatments are usually performed by staff members trained by doctors at either the University of Nevada Las Vegas or NOVA Southeastern dental schools. Most patients experience immediate, objectively measured improvement after the first treatment and, upon completion of the comprehensive rehabilitation, virtually all patients report continued satisfaction with their results.
The key to long lasting results from this therapeutic approach is harmonizing the rehabilitated musculoskeletal components with the force balancing of the dentition. Stabilizing the proprioceptive neurology through excellent dental treatment is accomplished after the rehabilitation is underway.
Implications for the dental practice
Relieving chronic pain symptoms in a drug-free and painless way is a significant attraction for a new patient that also creates new, high margin revenues from existing patients. Existing patients in the dental practice can immediately benefit from the technology, allowing instant revenue growth. Practices already capitalizing on this innovative approach estimate that more than 50 percent of their existing patients. Females, especially between the ages of 20 and 60, can benefit from the technology and rehabilitation techniques. Additionally, ensuring the longevity of elective and necessary restorations by establishing a functional dentomandibuar system can help patients commit to the other treatments they want or need.
Once fully trained in the proprietary assessment and rehabilitation protocol, practices can accept new patient referrals from other health care providers seeking drug-free solutions for their patients suffering from headaches and migraines. Physicians refer new patients, in part because of the unique assessment to AMA guidelines. For example, the ROM portion of the assessment process provides objective data to AMA guidelines. Incorporating this innovative technology and treating patients with chronic headache and migraine pain is proven to expand practices by providing an advanced level of total patient care. The complete system, combined with comprehensive training, positions dentists to achieve excellent patient outcomes to a new standard of care. When followed properly, this unique approach to addressing dentomandibuar sensorimotor dysfunction has been 93 percent successful in relieving symptoms of pain for properly diagnosed cases.
Additionally, because 80 percent to 90 percent of the examination and rehabilitation process is performed by dental practice team members, dentists can be more efficient in their use of chairtime and, therefore, the practice can realize greater profits. In fact, less than 120 minutes of doctor time is required for a multi-thousand dollar therapy case. Interestingly, most dentists who have implemented the TruDenta system report an average treatment plan of $3,500 to $5,000 per patient for therapy alone.
Conclusion
From assessment and examination through rehabilitation treatment, technology that has been used for years in sports medicine can now enable dentists to realize better patient care, increased doctor/team satisfaction, and new practice profits. By providing life-changing treatments that relieve patients of chronic pain and simultaneously establish a functional platform on which to incorporate elective or necessary restorations, dentists and their teams can expand their significance in their patients’ overall health.
References
1. Barnett ML. The oral-systemic disease connection. An update for the practicing dentist. J Am Dent Assoc. October 2006; 137 (Suppl 2): 5S-6S.
2. Ostler GL. Building professional referral relationships with physicians. Dental Economics. 2012. http://www.dentaleconomics.com/articles/print/volume-96/issue-12/features/building-professional-referral-relationships-with-physicians.html. Accessed July 3, 2012.
3.Sardella A, Demarosi F, Lodi G, Canegallo L, Rimondini L, Carrassi A. Accuracy of Referrals to a Specialist Oral Medicine Unit by General Medical and Dental Practitioners and the Educational Implications. Journal of Dental Education. 2007; 71( 4): 487-491.
4. Headache. US News and World Report. 2006. http://health.usnews.com/healthconditions/brain-health/headache. Accessed July 3, 2012.
5. National Headache Foundation. http://www.headaches.org/education/Headache_Topic_Sheets/Migraine. Accessed July 3, 2012.
6. American Dental Association. Dentists: Doctors of Oral Health. http://www.ada.org/4504.aspx. Accessed July 3, 2012.
7. Junge D. Oral Sensorimotor Function. Medico Dental Media International, Inc.: 1998.
8. Sessle BJ. Mechanisms of oral somatosensory and motor functions and their clinical correlates. J Oral Rehabilitation. 2006; 33:243-261.
9. Montgomery MW. T-Scan Dental Force Analysis for Routine Dental Examination. Dentistry Today. June 2011.
10. Cameron MH. Physical Agents in Rehabilitation, 3rd Edition. Saunders: 2009.
11. Öz S, Gökçen-Röhlig B, Saruhanoglu A, Tuncer EB. Management of myofascial pain: low-level laser therapy versus occlusal splints. J Craniofac Surg. 2010 Nov; 21 (6): 1722-8.
12. Marini I, Gatto MR, Bonetti GA. Effects of superpulsed low-level laser therapy on temporomandibular joint pain. Clin J Pain. 2010 Sep; 26(7): 611-6.
13. Srbely JZ, Dickey JP. Randomized controlled study of the antinociceptive effect of ultrasound on trigger point sensitivity: novel applications in myofascial therapy? Clin Rehabil. 2007 May; 21(5): 411-7.
14. Aguilera FJ, Martin DP, Masanet RA, Botella AC, Soler LB, Morell FB. Immediate effect of ultrasound and ischemic compression techniques for the treatment of trapezius latent myofascial trigger points in healthy subjects: a randomized controlled study. J Manipulative Physiolo Ther. 2009 Sep; 32(7): 515-20.
15. Zuim PRJ, Garcia AR, Turcio KHL, Hamata MM. Evaluation of microcurrent electrical nerve stimulation (MENS) effectiveness on muscle pain in temporomandibular disorders patients. J Appl Oral Sci. 2006; 14(1): 61-6.