Explaining new PPE and infection control protocols to patients
Explaining new PPE and infection control protocols to patients. Entire dental team should be on the same page while informing patients of new steps being taken to protect against COVID-19.
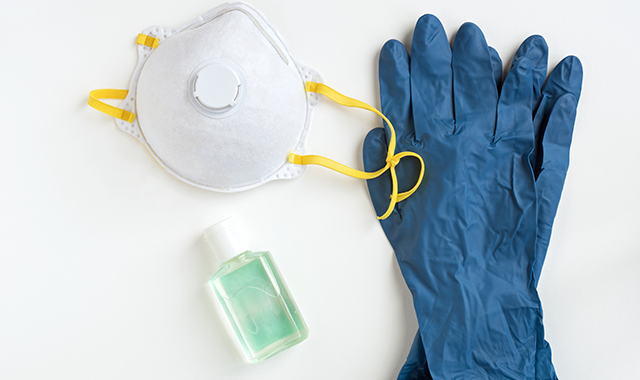
Under normal circumstances, the average person probably doesn't think twice about the types of PPE worn in the dental office. They have certainly seen doctors and hygienists in face masks and protective gloves-and there may even have been times where they saw someone wearing an N95 respirator or a gown-but really didn’t think to question why that specific piece of equipment was used.
After the COVID-19 pandemic, however, patients are sure to be more aware of PPE, infection prevention measures, and they may also be billed for equipment that they previously weren’t charged for-and they will have questions.
Concerns
PPE was hard to come by in the spring of 2020, so there was plenty of news and social media attention given to it. As such, patients are more aware of the need for protective equipment.
“Because patients have been viewing what health care workers are wearing in the hospitals when treating COVID-19 patients, I think it’s important for dental personnel to take special care when donning and doffing PPE in the presence of patients,” Mary Borg-Bartlett, President SafeLink Consulting, says. “For the most part, patients are now expecting to see what they are seeing on TV, and I think they will be more concerned if they don’t see similar PPE in the dental practice.”
Drawing attention to and explaining PPE is nothing new for dental healthcare personnel, but that may become more of the norm.
“Dental practices working with primarily a pediatric population has long been aware that children may need reassurance when receiving dental care,” Karen Daw, “The OSHA Lady”, speaker and consultant, observes. “Facial expression allows children to better understand emotions during social interactions. This is also true for adults. Think about which person you’d approach in a situation involving meeting someone new. Would you opt to have a conversation with someone with a smile or someone with a scowl? When a face is partially obscured by a mask, a dental professional knows that a smile can still be conveyed in the eyes. Now, with a respirator, full-length face shield, and isolation gown, our patients are seeking, even at a subconscious level, a way to put their minds at ease over unfamiliar sights. It may be difficult to convey that ease via body language or facial expressions so communication via email and phone calls, and consistent language from the entire team can help.”
Mitigation
PPE has, conventionally, only been visible in the operatory, but expect to start seeing it throughout the practice.
“Front office staff should wear a face mask as patients enter the practice,” Borg-Bartlett says. “This is the first visible change, along with plastic barriers or other markings, to keep physical distancing between the patient and the front desk personnel. As far as the clinical area, the only new items being worn are N95 respirators and face shields. The public has heard all about N95 respirators so they should be OK with these being worn. It may be necessary to explain to patients that the reason for the extra protection is due to this virus being airborne, and prior to COVID-19, the earloop surgical masks were sufficient.”
But it isn't just the PPE that will be a reminder of new infection prevention efforts. Expect more subtle (and not so subtle) reminders of infection control best practices.
“Another visual display of new infection control practices could be placement of instructional signs throughout the practice,” Borg-Bartlett says. “These are reminders, mainly to staff, to wear certain PPE or not to wear PPE in a particular area. A common poster is the Cover your Cough that is usually displayed in the waiting area and handwashing reminders in restrooms.”
Questions
Patient curiosity about PPE is nothing new, but it’s wise to anticipate questions.
“Even pre-COVID I coached practices to encourage safety dialogue with patients,” Daw says. “‘It’s nice to meet you, Mrs. Smith. I see you are here for an exam and cleaning. I’d like to share some things you might find interesting. For example, have you ever noticed the instruments used during your appointment are wrapped until you’re seated?’” This is a great springboard into all the things the practice does in the name of safety. Even though we know the instruments are sterilized and operatories are disinfected between patients, it’s an opportunity to plant that seed. This does multiple things: It answers questions the patient didn’t even know they had. It also allows them to think about the purpose of barriers, the use of PPE, and all that goes on behind the scenes to ensure their safety. I could ask an audience how many have ever been asked, ‘Do you throw your instruments away between patients,’ and the majority of them will raise their hands. That’s because the patient has part of the picture when it comes to what happens to those instruments between use. The other thing it does is reassure the patient they’ve chosen not just a good dental practice, but a safe one, as well. And in an industry where we rely on referrals and word-of-mouth, the safety conversation can pay dividends.”
“Patients are asking more questions now than ever before about PPE and infection control, so the dentist and staff must be prepared to answer patients’ questions,” Borg-Bartlett adds. “A good exercise in a huddle would be to role play. Pose this question that could come from a patient to staff members: ‘How safe do you feel working here?’ or, ‘Do you have any concerns for your safety?’ Dentists need to hear the answer the staff will give to a patient, and if staff does have concerns, address them right away. Dentists and staff need to be saying the same thing so patients aren’t confused if they receive differing answers or a staff member seems apprehensive to answer that type of question.”
Especially as practices reopen, questions are sure to arise, especially given what looks different and concerns for their overall safety. Practices need not wait for patients to come into the office to address these enhancements.
“Yes, the PPE is going to look a bit different,” Daw says. “If the practice has not been keeping up communication and is about to reopen, now is a great time to reach out. Think about what is going to be new for the patient and address that before they arrive. This can occur via an email broadcast to the listserv, or during confirmation calls. ‘Mr. Jones, we’re looking forward to having you back and seeing your smiling face again. Before you arrive, we want you to know we have taken every precaution and have implemented protocols that meet and exceed CDC guidelines. For your protection and the safety of others, we ask that you wear a clean mask or cloth facial covering for your appointment. When you arrive, just call, and Sarah will meet you at the car. She will conduct a temperature check and ask you the same questions I’m asking you today. She will then give you a bottle of hand sanitizer and we’ll need you to apply enough to cover front, back, and in-between fingers for 20 seconds. When you walk in, you’ll also notice that we have more personal protective equipment than before. This is designed to keep you, your family, and our dental family safe.’ However you say it, do it in the voice of the practice. A genuine and authentic style of communication will always win you brownie points.”
“Patients just want to be made to feel comfortable and safe, and that starts with the initial phone conversation when they are making an appointment,” Borg-Bartlett adds. “Front office staff should inform the patients what to expect when they arrive at the practice. Cover issues such as the patient’s temperature being taken, wearing a mask when they come to the practice, policies regarding companions, and then asking all the questions prior to them coming into the practice, including their recent travel to other countries or areas with a high prevalence of COVID-19; do they have a cough or are they experiencing shortness of breath or loss of smell or taste, and other questions recommended by the CDC.”
Surcharges
Between its scarcity and increased use, PPE is a more expensive component of dental operations. Paying for PPE is a new concern. Is it something that insurance companies will pay for or will that fee be passed down to patients? It depends on the practice’s policies and what insurance companies are willing to pay.
The ADA is encouraging third-party payers to adjust their fees to account for the increasing cost of personal protective equipment that dentists are using to protect themselves, their staff, and patients.
“Third-party benefit programs should either adjust the maximum allowable fees for all procedures or allow a standard fee per date of service per patient to accommodate the rising costs of PPE,” according to an ADA statement finalized April 21.
The ADA further advises dental practices to develop a consistent policy about PPE surcharges.
“Dentists should develop a standard office policy to document the additional PPE that will be used across all patients,” the statement reads. “This documentation methodology will justify a standard fee across all patients. Alternatively, dentists may wish to add a note in the patient’s record to document the details of PPE uniquely necessary for the visit when charging different fees based on the level of PPE used.”
Ultimately, the practices’ policies must be explained to patients, and practices should be ready with an answer.
“Some of my clients are charging a fee,” Borg-Bartlett says. “It ranges from $10 to $12 per patient. If a patient asks for an explanation of this surcharge, then explaining that it’s all about supply and demand and the supplies are low so suppliers are charging more, which has required the dentist to increase fees.”
Patients, likely, just took for granted that dentists, hygienists, and assistants wear masks and gloves. Going forward, they are likely to see more protective equipment (like face shields, gowns, and shoe covers). Patients are sure to have questions about that gear and they may also wonder if they're being charged for it.