De-mystifying the new Academy of Periodontology classifications
© Andriy Bezuglov/Adobe Stock

Debbie Seidel-Bittke, is the founder and CEO of Dental Practice Solutions, a leading dental practice management firm.

There seems to be a lot of confusion about the updated classifications for periodontitis.
Could this be that people resist change?
After all, the last time the American Academy of Periodontology (AAP) reclassified periodontal disease was 1999. It may be many years before the AAP makes a new revision so let’s embrace this change as it is here to stay.
Why The Change?
Since 1999 research has been conducted and did not address biological features between chronic and aggressive periodontitis.
The 1999 classifications emphasized disease severity and used other designations such as slight, moderate, and severe periodontitis.
Since 1999, it has been confirmed that a diagnosis based on severity alone represents a one-dimensional view of periodontal disease. The new AAP classification supports a multidimensional view of periodontitis, incorporating severity and potential tooth loss due to periodontology.
How To Use The New Classification1
The first step to use the new classification is to assess your hygiene patients and every new dental patient.
Patients must have an annual full mouth comprehensive periodontal exam (CPE).
The CPE includes all of the following:
- Pocket depths (six-point reading)
- Gingival recession
- Bleeding on probing
- Furcation status
- Mobility
- Suppuration/pus
- Mobility
- Plaque/biofilm
- Occlusion (Check patterns of wear)
- Up-to-date radiographs that show bone levels
- Fremitus
Also included are age, diabetes, smoking, cardiovascular disease, systemic diseases, etc.
Step Two: Determine the Stage2
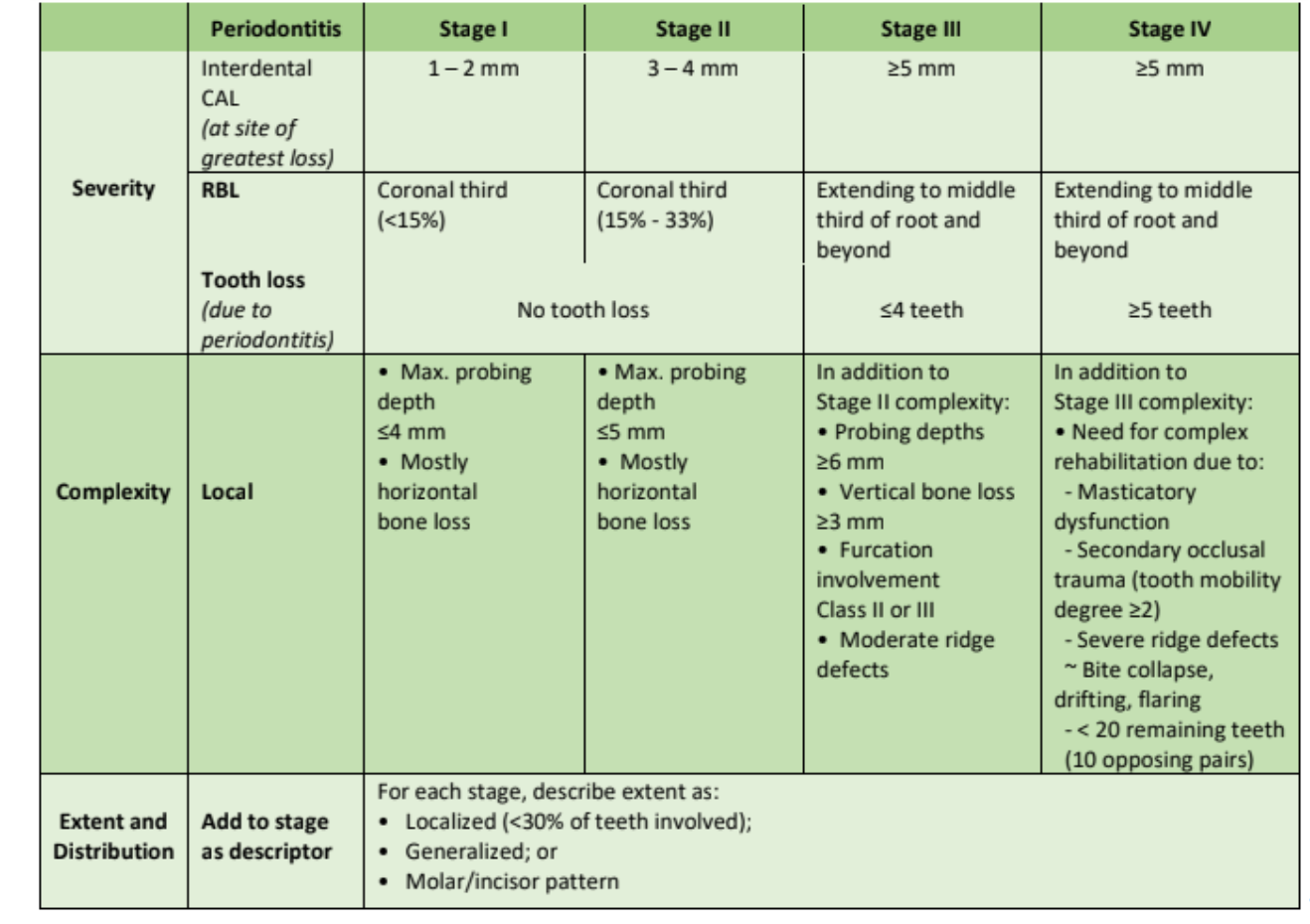
Next, review the stage chart above.
Move your eyes down the chart.
Example:
This patient has 3-4mm of clinical attachment loss. Maximum pocket depth is ≤5mm and only horizontal bone loss.
In this example, your patient will be Stage II Periodontitis.
Stage refers to the severity of the disease.
The severity of the disease includes clinical bone loss, radiographic bone loss, and even tooth loss due to periodontal disease.
Think stages of cancer.
Yes, we are talking about a patient’s oral health, however, when explaining periodontitis (“gum disease”) stage to your patient, it is more easily understood when you use the example of a patient who has cancer. Most people understand cancer has a specific “stage.” They have heard this term used before.
Always look at the complexity of periodontitis.
- Assess radiographic bone loss. Is it horizontal or vertical?
- Does the patient have occlusal issues that contribute to periodontal disease?
- The next step is to assess where the disease is located.
- Is the disease localized or generalized?
- Look at the molar and incisor patterns.
When you are assessing the stage of periodontitis, explain to your patient and show them what you “see.” Refer to the mouth/body connection as you explain inflammation to your patient.
This new classification provides a perfect opportunity to speak with your patient about the connection between inflammation in their mouth and inflammation in their body.
This is our opportunity as healthcare professionals, to share the mouth/body connection with our patients.
If a patient presents with a specific stage they typically will not change to an improved stage. Think of this as bone that does not grow back.
A possible conversation with your patient:
Example: Patient history. Mrs. Jones 40 years of age and a New Patient at this dental office. No medical conditions nor does she take any medications. Mrs. Jones smokes 2-3 cigarettes daily. Mrs. Jones will receive a full-mouth series of X-rays, a comprehensive periodontal exam, followed by a doctor exam. After the initial assessments are completed a diagnosis will be made. Both doctor and hygienist (together), during the patient exam, will come to a diagnosis for the patients’ condition.
Possible conversation prior to the hygiene patient-doctor exam: “Mrs. Jones, you heard me call out those numbers that were one through four and you heard me call out areas that are bleeding. The fours and bleeding that you heard me call out relate to inflammation and infection in your mouth.
We want to put a halt to this inflammation and infection because year after year inflammation and infection in your mouth contribute to inflammation in your body. Inflammation in your body contributes to other diseases such as heart attack, stroke, rheumatoid arthritis, Crohn’s, Alzheimer’s, diabetes, etc.
Very similar to when a patient has cancer there is a specific stage of cancer. The stage of cancer relates to the severity of a person's cancer. This is the same when a patient has gum disease. At this point, you have Stage II gum disease, and this means that you are in the early stages. When we treat gum disease at an early stage you have a good chance that the disease will not progress.
Once we treat the infection and inflammation you will need to return for routine preventive gum maintenance. At this stage of the disease, we can put a halt to the disease progression. This means less chance for tooth loss. When you reduce inflammation in your mouth you are less likely to have other systemic diseases that are related to inflammation. What questions do you have for me at this time?”
Next, after the hygienist talks with the patient (knee-to-knee and eye-to-eye), the doctor will complete an exam (with the hygienist present) and review X-rays taken at the beginning of the hygiene appointment.
Side note and important information to know: Notice that at the end of the conversation above, there was an open ended question. This allows the patient to ask questions and not answer with a “yes” or “no.”
Mrs. Jones’ radiographs show slight horizontal bone loss. Also, no carious lesions are present. No other significant findings were made during her appointment.
Step Three: Determine the Grade2
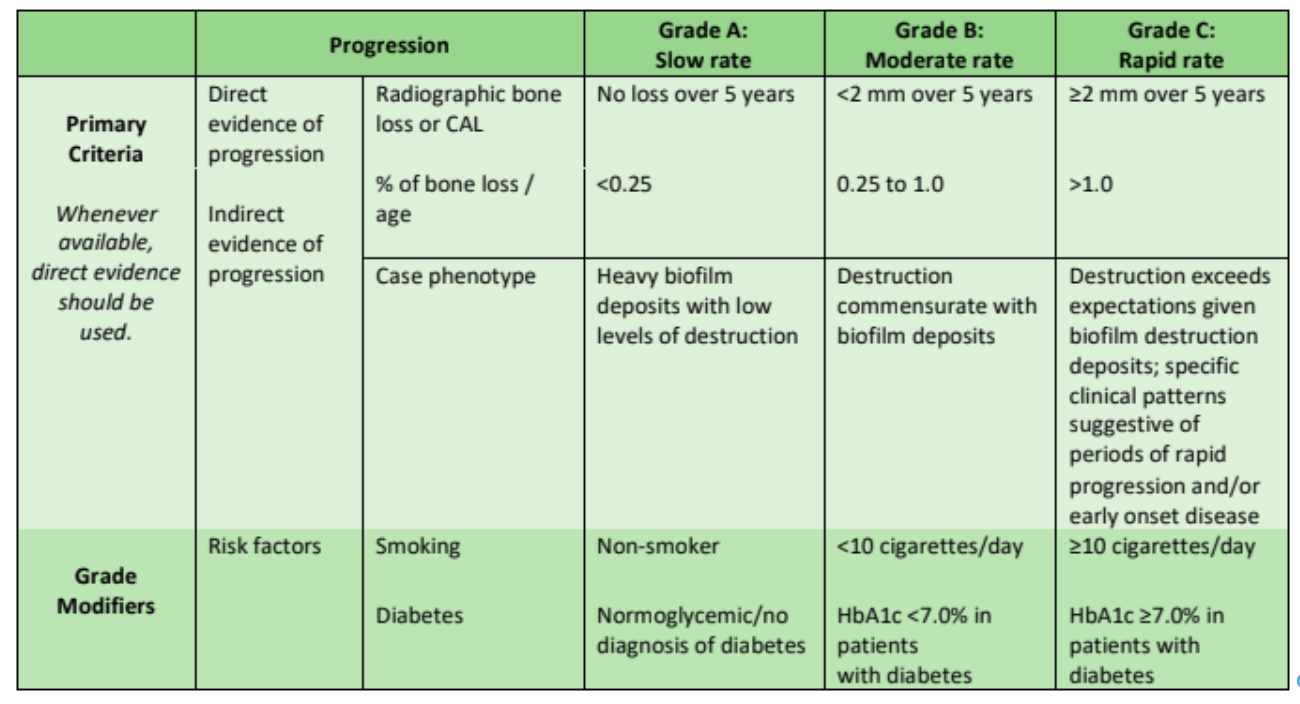
As you look at the grading chart (See above) you will assess which of these grades relate to the rate the disease will progress.
If you have a healthy patient; no radiographic bone loss nor do they have risk factors, you will not provide this patient with a grade.
It is a well-known fact that the number one risk factor for periodontitis is tobacco use. You will see on the grade chart above, that tobacco use is < 10 cigarettes daily and/or HbA1c < 7.0% with a diabetic. This means your patient is listed as Grade B (moderate rate). If your patient uses >10 cigarettes daily and/or HbA1c ≥7.0% with diabetes you will use patient C (rapid rate) as your grade.
If your patient stops using tobacco or uses < 10 cigarettes daily, their grade will change from rapid to moderate.
The one difference between staging and grading is that your patient’s grade can improve whereas the stage will rarely improve.
Each time your patient returns for maintenance you will re-evaluate the periodontal status and this includes assessing stage and grade.
Every time you evaluate your patient you will determine the following:
- Healthy patient
- Gingivitis patient—Localized: Slight, moderate, or severe
- Generalized—Slight, moderate, or severe
- Periodontitis: Slight, moderate, or advanced
A few important things to look at on the grade chart when assessing your patient are:
- Risk factors
- Radiographic bone loss (RBL)
- Phenotype3
Use the Stage and Grade in Your Daily Practice
Each day, dental hygienists see areas of inflammation in their patients’ oral condition. Never before have we had so many opportunities to share the mouth/body connection.
In the above situation, Mrs. Jones is a stage II localized slight periodontitis. Due to her use of < 10 cigarettes daily her grade will be B.
Example of clinical notes:
Stage II localized perio. Grade B due to tobacco use, < 10 cigarettes daily.
Notice that the chart notes are not long. Make this simple to use in your chart documentation. If you have templates for your clinical notes, use these to make this easier, not more difficult to record.
Conclusion
Dental professionals have gained more knowledge about the mouth/body connection over the past 20 years. Dental hygienists no longer “just clean teeth.” Now is the time to embrace the small changes that occur like the speed-of-light in our dental world.
It’s time to embrace these changes. It’s time we work together, using the knowledge, the research, and the tools at our fingertips that allow our patients to live healthier and longer lives.
Will you partner with me to help share this message about optimal oral health leading to improved health and a longer life? When we embrace this message and find a way to diplomatically and professionally share this, we can help put a halt to the disease process.
References
1. Proceeding From The 2017 World Workshop On The Classification Of Periodontal And Peri-implant Disease And Conditions - a. Please refer to: http://bit.ly/AAP2017Proceedings
2. Please refer to: http://bit.ly/stagegradechartAAP
3. J Periodontol. 2018 Feb; 89(2): 166–175. - a. Please refer to: http://bit.ly/AAPPhenotype