Chill Out: Managing Infection Control in the Heat
Keeping both patients and employees comfortable in a practice while still maintaining infection control protocol is possible.
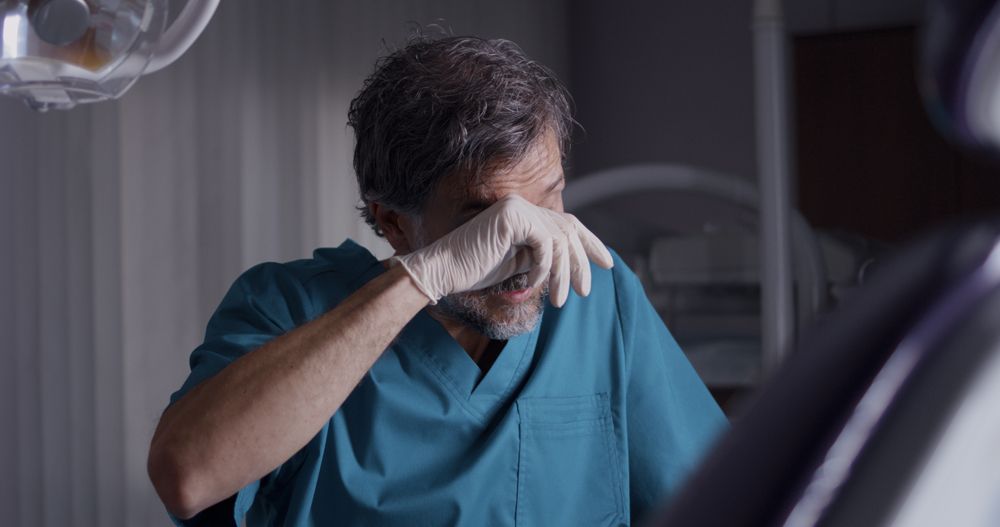
Chill Out: Managing Infection Control in the Heat. Photo courtesy of Framestock / stock.adobe.com
Last week, my wife was getting ready for a dental appointment, and she said, “It’s hot outside, but I’m going to bring a sweatshirt, because they always keep it so cold.”
“There’s a good reason for that,” Karen Daw, “The OSHA Lady”, speaker and consultant, later told me. “Team members wear so much personal protective equipment (PPE) that they have to keep the air conditioning turned up to keep themselves comfortable.”
In the summer months, practices must contend with several environmental challenges – including heat, humidity, and air quality – to keep themselves comfortable and their patients safe.
Balancing act
Finding the temperature that’s right for everyone – clinical staff, front desk staff, and patients – can be somewhat of a juggling act.
“What can we do to make the clinical team comfortable,” Daw says. “And 1 of the first things I like to suggest is, can we make it cooler in the office, in general? And then I get team members saying, ‘But, the doctor doesn’t want it too cool, because the patients complain. What can we do to resolve that?’ Why don’t we manage expectations? What if, during the text, email or phone confirmation, we let our patients know, ‘Hi, Mr. Smith, we’re looking forward to having you back in our office for your dental cleaning, and by the way, we’re following the high standards of safety in our practice for your benefit and the benefit of our team members. As a result, you may notice it a little bit cooler in our practice than you’re used to. So, we’re recommending to just bring a light jacket for your appointment.’ What if we did that? And then we could make everyone happy and we’re managing those expectations ahead of time.”
PPE
PPE exists to keep everyone safe, but that equipment can become uncomfortable and potentially hazardous to use in warmer temperatures.
“If your goggles are fogging up when you’re wearing a mask, it means that your exhalation air is escaping. Be sure to crimp the nose band of your mask securely” infection control consultant and speaker Leslie Canham, CDA, RDA, says. “I know, for myself, if my N95 respirator is not sealed properly around my nose, when I exhale, my regular glasses fog up. This means that my PPE doesn’t fit well.
“Many times,” she continues, “we have 3 people in a treatment room – the dentist, an assistant, and the patient – and they’re all in close proximity to one another. In addition, an overhead light may give off a little heat, as well.”
PPE does not need be stifling. Team members can still wear appropriate PPE with an element of comfort in mind.
“You can wear blue jeans and a t-shirt for all OSHA is concerned,” Daw says. “It doesn’t matter, because you’re putting on PPE over them once you get into the workplace. That PPE cannot leave the workplace. So, what can you wear underneath it? Do you have to wear scrubs underneath it? I know of dental offices that have gone with the scrub pants, but as far as the top goes, they switched to wicking runner tops, for example – something that kind of wicks away moisture from the body and helps to regulate your temperature a little bit more, so that it is a little bit more comfortable underneath that gown and other PPE. It doesn’t matter what you have on underneath that, as long as your PPE on the outside protects your skin and the clothing underneath from contamination or exposure.”
Not just comfort
Ensuring that team members are comfortable is an important consideration, but there are safety concerns that go hand-in-hand with the right temperature.
“It can present a problem when temperature is crucial in certain circumstances,” Canham observes. “For example, some dental materials are adversely affected by temperature.”
Further, some PPE is impacted by environmental extremes.
“Exam gloves, and other disposable items, can be affected by heat and humidity,” Canham says. “It’s a good idea to store these items, especially exam gloves, away from extreme heat, direct sunlight, or sterilizers. For example, the steam from an autoclave can cause damage.”
Team member wellbeing is important not just from a comfort standpoint, but also as a safety concern.
“You add the extra steps of extra physical exertion, along with the extra PPE, and we have team members who are really getting hot and at risk,” Daw observes. “They might not be as attentive or they’re just uncomfortable. And when they’re not comfortable or if they’re sweating all over the place, then their minds are elsewhere. ‘Gosh, I am just super hot.’ We could, potentially, be at increased risk for injury in the workplace. What can we do to make our team members comfortable? Because certainly, if it’s too warm, it could increase the possibility that somebody might stick themselves with contaminated instruments or they might skip a step in infection control, because their mind is not on the task at hand.”
It’s also valuable to build some breaks into team members’ days.
“My recommendation is to take breathing breaks from your PPE throughout the work shift,” Canham advises. “Stay hydrated and perhaps even stock up in the staff lounge refrigerator with some electrolyte drinks to replenish if you are getting dehydrated during your workday.”
“A good work practice control might be to give your team members breaks,” Daw adds. “Maybe a little bit more frequent breaks, especially if they’re wearing N95s and you’re breathing through a filtering facepiece respirator all day. And just being mindful of, ‘What can we do to make our team members comfortable’.”
In the air
Air quality concerns are also important considerations. Between SARS CoV-2 (the virus that causes COVID-19) and the effects of wildfires, practices find themselves ensuring that the air is safe to breathe. Some may opt to use a fan to circulate air. For some, the use of a fan may be confusing.
“A common question I get is whether or not fans are allowed in the operatory because of the concern around aerosols,” Daw says. “And what’s interesting is that I have not found anything specific by the Centers for Disease Control (CDC) or OSHA that specifically states that you cannot have a fan. A lot of our team members use fans so they can stay cooler. And there’s no actual infection control literature that says, ‘No, you can’t do it.’ It could circulate aerosols, and therefore, may be discouraged, but and there is nothing that outright prevents it.”
Where the fan is placed does matter, especially as infection prevention is concerned.
“With SARS-CoV-2, air movement must be in a clean to less-clean direction, to reduce the distribution of contaminants,” Canham says. “The CDC recommends the use of air purifiers, or portable high-efficiency, particulate absorbing air filtration systems – or HEPA filters – while patients are undergoing treatment. I purchased an air purifier for my home, and I found that it does help cool my room. CDC highly recommends that you consult with your heating, ventilation, and air conditioning system technologist or consultant to help you understand clinical air flow patterns and determine air changes per hour. In addition, they can investigate increasing filtration efficiency to the highest level compatible with the HVAC system, without significant deviation from designed airflow, and investigate the ability to safely increase the percentage of outdoor air supplied through the HVAC system. Ultimately, a properly functioning HVAC system can provide safer air quality and be very helpful for maintaining a more comfortable temperature.”
HEPA air filtration units don’t have to be just be located in treatment areas.
“I like to see them in the reception room of a dental practice. I believe that it conveys a strong message to the patient about infection prevention and safety,” Canham says. “With SARS-CoV-2 being an aerosol transmissible virus, patients understand that we care about their safety in the reception room as much as we care about their safety in the treatment chair.”
Proper environmental levels in the dental practice are certainly important, but not just from a comfort standpoint. PPE, chemicals, and equipment need the right levels of heat and humidity to work properly. That’s not to negate the importance of comfort. Team members work better when they’re not distressed, and they’re less likely to make potentially hazardous mistakes.