Addressing Suicidal Tendencies in the Healthcare Population
Dentists and other healthcare professionals have been known to be at an increased risk of suicide due to high-pressured careers. A recent report from the CDC shows the nationwide rates of suicide and discusses what can be done to arrest this alarming epidemic.
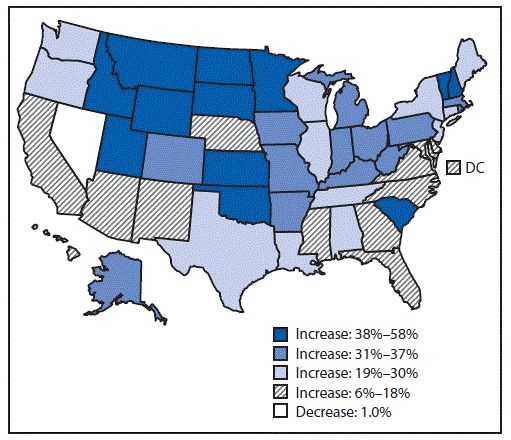
Percent Change in Annual Suicide Rate by state - United States, from 1990-2001 to 2014-2016
SOURCE: Centers for Disease Control and Prevention - Vital Signs: Trends in State Suicide Rates — United States, 1999—2016 and Circumstances Contributing to Suicide — 27 States, 2015
Mental health conditions and life stressors are contributing to a rise in suicide rates in the United States, according to a recent report from the CDC.
In every state except Nevada, where suicide rates have been consistently high, there has been an increase in the number of suicide deaths from 1999-2016, with a 30% or higher observed rate increase in 25 states.
Dentists, physicians and other healthcare professionals frequently rank among the most at-risk occupations based on historically high statistical rates of suicide. A study published in Psychological Medicine contributes the higher rates among these groups to easier pharmaceutical access. The same study, however, acknowledges a drop in the prevalence of suicide deaths from 1979 — 2005 for veterinarians, pharmacists, dentists and physicians in the United Kingdom where the study was conducted. Researchers credit relative economic prosperity in early 2000s as a possible driver behind the positive change.
Among white males, who represent the highest risk demographic, dentists today are 70% more likely to commit suicide than the average population, according to data published by New Health Guide. The fluctuation in suicide rates and its prevalence within the healthcare sector is alarming. Recognizing stressor events that initiate suicidal tendencies in dentists, healthcare professionals and the general population is important for reducing future outcomes.
Stressor events commonly attributed to suicide include relationship problems with a significant other or family member, legal problems, eviction, financial setbacks and health complications. The recent CDC study links both victims with and without known mental health conditions as experiencing significant life stressors, but those without known mental health conditions had a higher likelihood of experiencing these problems.
A significant portion (about 50%) of individuals with mental health conditions were receiving active treatment when they died, suggesting that more effective, accessible and affordable modes of treatment are necessary for a population base that is already suffering from problems that might accelerate the likelihood of suicidal thoughts.
The consensus surrounding suicide prevention is that it’s a multifactorial issue — mounting stress from several life circumstances leads to most cases. Even with this insight, most prevention resources are focused on mental health conditions, even though the data shows about half of suicides are committed by victims with no known history of mental illness. Identification of suicidal tendencies in the general population is difficult, yet there needs to be a shift in suicide prevention resources to include all at-risk persons.
Some prevention strategies could offer support to those with suicidal thoughts, including a more robust system for economic support, easily accessible means for learning about coping skills and resources for connecting to social networks. Some states, like Colorado, are developing a better understanding of and effective approaches to suicide prevention and are implementing programs for citizens who need help.
The CDC recommends statewide suicide prevention programs be implemented to address a scope of issues that lead to suicide deaths. Awareness of personal stressor events is important to all professions and demographics in the fight against rising suicide rates.
Healthcare professionals continue to be a vulnerable sector of the population. High-pressured careers coupled with the stresses of everyday life can possibly heighten feelings of hopelessness for individuals with or without a history of mental health conditions. Dental providers are trained to focus their attentions on the health of their patients and frequently neglect their own needs, leading themselves to feel burned out, or even anxious and depressed.
The following tips taken from a study in the International Journal of High Risk Behaviors & Addiction are important to keep in mind when it feels like there is nowhere to turn:
- Problem-focused strategies of coping with stress and anxiety are less effective than emotional-focused (resolution) strategies.
- Avoidance or defensive strategies to stress, anxiety and depression may aggravate suicidal feelings. These include negative, wishful or “what if” thinking, drug use, disengagement and denial.
- It is important to reach out for emotional support from a social or familial connection.
- Remember that suicidal thoughts are fleeting and do not require action.
- Ask for help. State organizations for suicide help can be found here.
Dental and healthcare professionals are poised to be instrumental in the detection of anxiety and depression in local communities. Personal care must be achieved before the needs of others can be addressed.
Click here to sign up for more Dentist's Money Digest content and updates.RELATED:
More Coverage on
- Study Finds Link Between Sugar and Common Mental Disorders
- Reduce Stress and Rediscover the Passion of Dentistry
- The Most and Least Stressed Cities in the U.S.