5 fascinating questions dental hygienists asked Kara RDH in January
As a well-known and accomplished dental hygienist, Kara Vavrosky often gets asked for advice. Here, Vavrosky shares five more interesting questions she's been asked recently, along with her answers.
As a well-known and accomplished dental hygienist, Kara Vavrosky often gets asked for advice.
She runs the popular Facebook page Dental Hygiene with Kara RDH and is also the founder of dentalhygieneanswers.com, a question-and-answer platform for dental hygienists.
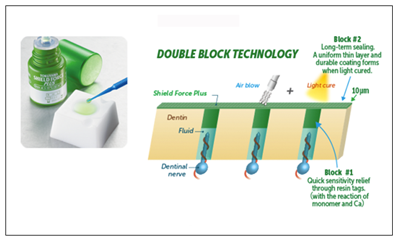
SPONSOR MESSAGE
Reduce tooth sensitivity and pain in your patients with Tokuyama's innovative Shield Force® Plus light-cured desensitizer. Offer them both instant and long-term relief with its exclusive Double-Block Technology. Click here to learn more.
Here, Vavrosky shares five more interesting questions she's been asked recently, along with her answers.
Continue to the next page to view our slideshow of these questions and answers.

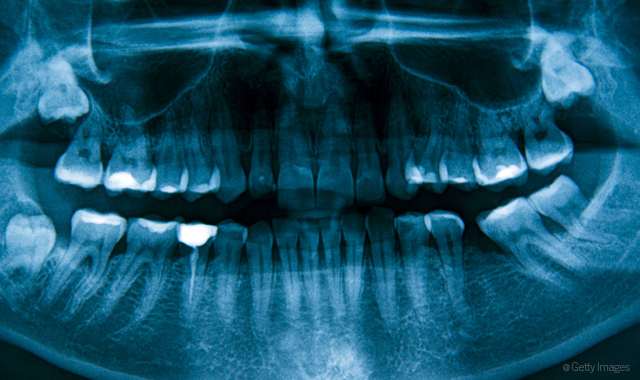


What do you tell a patient who asks how much radiation is given during routine X-rays?
First, I explain how there is much less radiation using digital radiographs than traditional. I like to state why radiographs are needed (we are working blind without them). Then, I like to give the patient examples of comparisons. For example, four bitewings equal 79 times less radiation than a year of background radiation from the environment. Four bitewings equal 0.5 mrem of radiation. In comparison:
- Flying in a plane is 5 mrem
- 1 mrem/year from a smoke detector
- 10 mrem/year cooking on natural gas stove
- 10 mrem/year living in a brick house
- 36 mrem/year smoking a pack of cigarettes per day
- 2 mrem/year sleeping next to your spouse
Even eating a banana gives you more mrems than dental X-rays!



Is it safe to do SRP during pregnancy (second trimester perhaps?) or should you wait until the patient has the baby? What are some of the contraindications?
The American Academy of Periodontology and the American Dental Association both state the importance of maintaining oral health throughout pregnancy. Research is beginning to show a correlation between periodontitis and pre-term and low birth weight babies. The best course of action is to have a release from the patients OB/GYN stating treatment is safe and which local anesthetic can be used (they might recommend no epi).
I did read an anesthesiologist’s view on the use of local anesthesia during pregnancy and she stated that given that 1) The amount of anesthetic is extremely diluted by the time it redistributes in the body, and 2) The placenta isn’t functional for most of the first trimester so there is no direct highway for drug transfer yet, and 3) Your body completely breaks down the drug in a matter of hours and 4) The baby’s relatively acidic body environment (compared to your body) makes it much harder for the LA to enter its cells.
All these things add up to negligible exposure for the baby, and even if there is exposure, the baby’s blood cells and liver and kidneys break it down. Further, all LA does is temporarily block sodium channels on the surface of cells that are important for the transmission of pain signals. And the medicine in epidurals is the same as local anesthesia. The only risk I found is the normal risk of allergic reaction regardless of pregnancy or not.



What age do you start spot probing?
What age do you do a full perio chart?
Do you believe probing introduces harmful bacteria into the sulcus?
Due to the fragility of the periodontal ligament in an erupting tooth, I begin doing a full perio chart on patients 16-18. The deciding factor for me is homecare, plaque/calculus amounts, health of gingiva (if gingivitis or even perio is present probing is indicated), etc. Of course this is all dependent on the patient, not a “cookie cutter” protocol. I perio chart every patient 18 and older once per year, sometimes twice per year if they are perio maint.
I try not to only spot probe because of one patient situation I encountered. The patient had impeccable homecare, who alternated with the periodontist and general dentist for cleaning every three months, but due to severe clinching and possible fractured root, I found a 9 mm pocket (no bleeding present). The rest of her readings were 1-3 mm. If I had only spot probed I would have missed it! Big lesson for me! I don’t think probing introduces harmful bacteria into the sulcus any more than scaling, brushing or flossing does.



Is it normal to be nervous to give injections?
I have been a RDH for just over a year now, and I still am nervous to give injections, is this normal? I have been successful getting my patients numb but am still nervous when I see NSPT or SRP on my schedule. As an RDH, when did you start to feel really comfortable with these procedures?
The first office I worked in was very high volume in which the doctor saw on average 50-70 patients per day (don’t even get me started on how unethical this is – I am not there anymore!). I anesthetized many patients for him throughout the day, like upwards of 20-30 patients per day – multiple injections per patient. Needless to say, I am extremely comfortable giving injections now! Mind you, when my own blood is drawn, I have been known to pass out.
So my point here is practice will make you comfortable!I was nervous at first too, but you need to dive in and get practice under your belt, to slowly become more confident. If you have time in your schedule, anesthetize your doctor’s patients for practice (if this is allowed in your state). Or even peek over your doctor’s shoulder when he/she anesthetizes. Remember your schooling and don’t hesitate to look through your anesthesia books once in a while, especially if they came with a CD. Also, check out YouTube for injection techniques. Be confident in your skills, you got this!


Patients that tighten their lips
Other than cotton rolls, what do you do for people to tighten their lips/tense their chins? I have a patient that is so bad, even with cotton rolls, when I’m cleaning the mandibular anteriors, his lower lip goes over the incisal and blocks my vision.
This not only because it makes it hard to work, but it’s actually dangerous to both you and the patient due to sharps injury possibility. I had a patient nick their own lip with the ultrasonic because of doing this. Let me tell you that was a lot of blood! I have patients like this hold their own lip out of the way. If that doesn’t work, I have them hold a mirror with one hand and their lip with another to show them what they are doing. Sometimes telling a patient to smile or bite on the saliva injector will cause their mentalis muscle to relax. When all else fails I tell them that I will need to anesthetize them (left and right incisal) if they can’t relax. Needless to say, I’ve never had to anesthetize someone because that gets their attention!