Test your dental implant IQ
As the population continues to age, more patients will turn to implants to replace missing teeth rather than ill-fitting dentures or partials. These patients are more educated about implants than ever before, and they’re excited about the possibilities they offer, from a more confident smile to the ability to eat with no pain or discomfort.
As the population continues to age, more patients will turn to implants to replace missing teeth rather than ill-fitting dentures or partials. These patients are more educated about implants than ever before, and they’re excited about the possibilities they offer, from a more confident smile to the ability to eat with no pain or discomfort.
But there’s a lot you need to learn before you can successfully implement implants into your practice. Not only do you need the proper training, you need to stay up-to-date on the latest products and techniques designed to make implant placement more predictable and effective.
Once you dedicate the time necessary to hone your skills and obtain the knowledge you need to successfully place implants, you’ll not only be able to offer patients a service that improves their quality of life, this new skill will renew your passion for dentistry and increase your practice revenues.
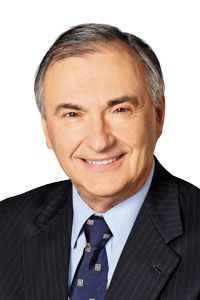
To help you learn more about dental implants and the benefits they can bring your patients and your practice, we reached out to implant experts and asked them to answer a set of true/false questions. The experts offer insight into why these questions are true or false, and hit on a variety of implant-related topics from who should be placing implants, to how CBCT technology can improve diagnosis to the benefits of new cement-free solutions. The questions were submitted by DPR’s Chief Dental Editor Dr. John Flucke, his associate Dr. John Huebner, the Academy of Osseointegration and dental implant manufacturers.
Free on-demand webinar: Understanding medical billing and its relationship with 3D
Before reading the responses, take a look at the true/false questions and test your implant IQ. See how many questions you can answer correctly, then check out what the industry experts had to say.
The questions:
-All GPs should be surgically placing implants.
-Mini Dental Implants can be a great option for edentulous patients.
-CBCT technology can help improve diagnosis and make treatment planning more predictable.
- Cement-free solutions offer enhanced flexibility and reduce the risk associated with cement excess.
- Maxillary anterior single-tooth implant restorations are easy and could be a good place to gain experience with dental implants.
- Edentulous patients' first choice of care, if possible, may include an implant assisted 2-implant mandibular overdenture.
- The proximity of an implant to a tooth or another implant is not important.
- Implant crowns in the posterior always should be splinted if there is an adjacent implant present.
- Every implant case should be done using a surgical guide.
- Every implant case should be done with a 3D scan as part of the treatment planning process.
- Implants can only be immediately loaded when splinted together in a full arch prosthesis.
- Occlusion for an implant crown should be the same as that of a crown on a natural tooth.
- Socket preservation has no effect on the eventual success of an implant and its prosthesis.
- GPs don't really need much training to begin placing implants in their practices.
- Mini implants are equivalent to larger root form implants in reliability and functionality.
Category Cruncher: The importance of implants
Continue to Page 2 to read what dental professionals had to say about the above statements ...
1. All GPs should be surgically placing implants. False.
: Not all GPs should be placing implants. The only GPs that should place implants are those willing to put in the time and finances necessary to acquire the education and skills they need to place implants properly. You need special equipment, special knowledge and to dedicate a sufficient amount of time to get that knowledge and sharpen your skills to perform these procedures for your patients. It’s not something anybody can do. It takes a dedicated person.
Once you have the proper equipment and education, you also need to look at the nature of every case. Not all cases are the same. There’s a huge difference between placing an implant in an area that has sufficient height, width and bone, and treating someone with a severely resorbed jaw in need of reconstruction with a bone graph. You have to be honest with yourself and only perform cases within your skill level.
2. Mini Dental Implants can be a great option for edentulous patients. True.
Karen Capiz, U.S. Marketing Manager, Implants Portfolio, 3M ESPE Dental: 3M™ ESPE™ MDI Mini Dental Implants are a great option for edentulous patients. As dentists know, edentulous patients often suffer from a loss of bone structure and ridge resorption in the jaw. With 3M ESPE MDIs, patients need just 4.8 mm of bone tissue width for successful integration, which is significantly less than the bone mass required for success with traditional implants.
Related reading: How the general practitioner has been critical to the future of implant dentistry
MDIs also can be placed much quicker than traditional implants and have a much shorter recovery time. Because MDIs are self-tapping, auto advancing and generally very narrow, dentists can often place them without cutting a flap or performing a bone graft. Placement can occur with the dentist simply drilling a small pilot hole to perforate the cortical bone and then screwing the implant into place.
With no need for a bone graft or time to allow osseointegration (MDIs are designed for stability in soft and dense bone), MDIs often can be loaded immediately after placement and require minimal to no recovery time, which is a significant benefit to patients and dentists – especially for the elderly or those with compromised health.
Many long-time edentulous patients have extremely ill-fitting dentures and a poor quality of life. In one day, this procedure offers immediate stabilization, allowing patients to resume normal eating habits and regain the confidence to speak and smile normally.
Cost is another consideration. MDIs can be a more affordable treatment path, and at times costs patients have as much as traditional implants.
It’s of course important to consider every patients’ individual needs to determine what options are best for their long-term health – but MDIs offer an affordable solution that requires less bone mass, a less invasive procedure and less recovery time, a combination that makes them a good treatment option for edentulous patients.
Related reading: How technology can simplify the placement of dental implants
Continue to Page 3 to further test your implant IQ ...
3. CBCT technology can help improve diagnosis and make treatment planning more predictable. True.
Dr. Justin Moody: With CBCT technology, I gain an added perspective into a patient’s specific dentition that allows me to achieve accuracy and to avoid potential surgical and restorative complications. The images support my ability to diagnose, plan and treat. Knowing the precise data on such aspects as buccolingual dimensions, concavities, bone height, and anatomical anomalies brings me great confidence before, during and after surgery.
My CBCT scanner, i-CAT, features software tools to help me proceed from surgically placing the implant and abutment to final restoration. I also can combine 3D images with intraoral scans for a comprehensive representation of the hard and soft tissues.
Not only does my i-CAT provide information that helps me establish diagnosis and implant placement plans, this imaging modality also offers many great benefits to my patients. The new Smart Scan Studio Simulator’s presentation option helps them better understand why I am choosing a certain path of treatment. Therefore, they may be more willing to accept my treatment plan, and be more compliant with my treatment recommendations.
With all of the advantages that i-CAT affords my implant practice, I would never consider going back to a 2D practice. I live in a 3D world now.
Related reading: Highlighting narrow diameter overdenture implants
4. Cement-free solutions offer enhanced flexibility and reduce the risk associated with cement excess. True.
: Cemented implant restorations were introduced as a way to manage esthetics and occlusion when dealing with implant angulation issues. They also provided the team (dentist and technician) with techniques and processes they were familiar with, namely cement-retained restorations.
Tooth-supported cemented restoration have existed for more than 100 years with few, if any, related biological issues. However, the same cannot be said when it comes to the cemented implant restorations.
Cement excess can elicit adverse soft tissues responses ranging from inflammation, increased plaque accumulation to peri-implantitis and its associated bone loss-which ultimately can result in implant loss.
Fragile soft tissue (hemidesmosomal) attachment to the implant, subgingival margin placement, poor control of cement flow and inappropriate cement use all contribute to an increased likelihood of peri-implant disease.
Several academies (including the American Academy of Periodontology, the American Academy of Restorative Dentistry and the Academy of Osseointegration) as well as numerous high evidence systematic reports have found implant restorations have fewer biological issues when a screw-retained restoration is used rather than a cement-retained restoration.
New innovations, such as the Angulated Screw Abutment from Nobel Biocare, not only provide a biologically friendly solution, they also address implant angulation issues. Esthetics and occlusion are easier to control, enhancing the flexibility of the screw-retained restoration and reducing the risks associated with residual excess cement.
Related reading: Nobel Biocare launches new, complete, cement-free posterior solution at IDS 2015
Continue to Page 4 to further test your implant IQ ...
5. Maxillary anterior single-tooth implant restorations are easy and could be a good place to gain experience with dental implants. False.
: This region and restoration requires significant attention to multiple details in treatment planning and delivery of care. Considerable skill and experience are necessary to address functional as well as difficult anatomical and esthetic factors the treating dentist can easily overlook or under appreciate. Treatment planning is critical and relies on the pre-surgical work-up, including the clinical and radiologic examinations.
Clinicians may be confronted with tissue deficiencies caused by various conditions. Such deficiencies may require bone augmentation procedures such as onlay grafts or guided bone regeneration (GBR) techniques, which may use simultaneous or staged approaches to regenerate adequate volumes of bone for implant placement. Soft tissue handling, precise implant placement, a restorative driven 3D approach and adequate follow-up are among challenges clinicians face.
Successful implant surgeons working in the esthetic zone have a sound biologic knowledge of the hard and soft tissues and the anatomy at the implant site, a thorough surgical education and sufficient surgical familiarity with esthetic implant placement.
This treatment requires experienced and seasoned clinicians for both surgical and restorative treatments as well as collaboration with an excellent dental laboratory. This team approach minimizes the potential for complications and maximizes the benefits for our patients and the entire implant team.
Related reading: Sterngold reveals new implant system
6. Edentulous patients' first choice of care, if possible, may include an implant assisted 2-implant mandibular overdenture. True.
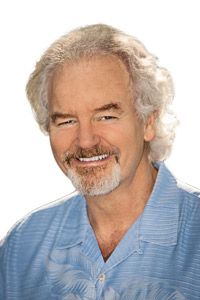
Dr. Russell Nishimura, President of the Academy of Osseointegration: Many studies have documented the multiple benefits, efficacy and long-term results implant overdentures provide in the lower jaws. The increased support, stability and retention leads to greater patient satisfaction, comfort and confidence. This treatment dramatically reduces the number of patients once considered “problem denture wearers.”
Without dental implants, patients may not be able to adequately control their dentures during speech and mastication, and their residual ridges may not be able to withstand the functional forces dentures place on their oral tissues. Clinicians may find the fabrication of an overdenture is facilitated by stable and accurate records implants provide. This leads to predictable results, improved stability and retention, as well as enhanced speech and esthetics.
The 2-implant mandibular overdenture is probably the greatest value in implant dentistry for patients. It can replace a whole arch of missing or failing teeth and provide improved function with minimum surgery and expense. The anterior mandible has demonstrated the highest success rates, and there are multiple methods to retain the 2- implant overdenture. This includes bars with clips, ball attachments and the Locator attachment.
The mandibular overdenture is a well-documented and established treatment modality, and some clinicians consider it the standard of care for elderly patients.
Bench Mastery: Kahng on an ideal implant bridge (Video)
Continue to Page 5 to further test your implant IQ ...
7. The proximity of an implant to a tooth or another implant is not important. False.
: I might agree with this statement, if it ended with “as long as it is at least 2 mm from an adjacent tooth and 3 mm from an adjacent implant.” There are two primary considerations driving the recommendation concerning proximity to teeth and implants: Biologic and restorative.
The biologic consideration relates to the need for a zone of supracrestal attachment around the implant-abutment interface. It is a similar concept to the biologic width around teeth, which mandates restorations be no closer than 2 mm to the underlying bone to prevent inflammation.
With implants, the dimension is smaller, mainly because of the lack of perpendicularly inserting gingival fibers. Without “platform switching”-moving the edge of the abutment in from the edge of the implant-this dimension seems to average about 1.5 mm. With platform switching the dimension of the implant biologic width decreases to less than 1 mm. So, the biology of the gingival attachment of implants leads the surgeon to place implants no closer than 3 mm to one another without platform switching and no closer than 2 mm with platform switching.
Fortunately, the restorative considerations do NOT significantly complicate the biologic considerations. For most implant systems, fixture-level impression posts are generally no wider than the width of the implant plus 1.5 mm. The expectation that the restorative process will be simpler with 3 mm of clearance between adjacent implants “trumps” the biologic potential to have implants within 2 mm of each other with platform switching, leaving us with a uniform “3 mm” recommendation for separation between adjacent implants.
Likewise, even though the biologic width for platform switching implants suggests an implant could be placed within 1 mm of an adjacent tooth, restorative simplicity argues in favor of 2 mm of separation.
Related reading: Unpacking important implant system and fee data in dental practices
8. Implant crowns in the posterior should always be splinted if there is an adjacent implant present. False.
Dr. Brien Harvey: The maxim that posterior implant-supported crowns should be splinted dates back to the ‘bad old days’ of early implant designs, such as external hex implants that had poor resistance to abutment micromovement under stress, with the resultant expectation that abutments screws-and therefore the prostheses-would loosen over time. Splinting multiple implants together dramatically reduced the micromovement of the abutments and thereby reduced the tendency for prostheses to come loose.
“Modern” implants, incorporating internal attachments, frequently including a conical connection between the implant and abutment have become the norm over the last 10 years or so, while we should acknowledge the pioneering internal conus designs stretch back 20+ years. The improved stability of the implant-abutment interface make it possible to use “permanent” cement on single implant crowns with predictably favorable long-term results.
The significant and predictable reduction in abutment screw loosening, resulting in long-term restorative stability for single-tooth implant-supported prostheses, argues strongly AGAINST splinting posterior implant-supported crowns to leave the patient with “single tooth” dentistry, thereby facilitating the process of effective oral hygiene.
Related reading: How is REALLY looking for dental implants information?
Continue to Page 6 to further test your implant IQ ...
9. Every implant case should be done using a surgical guide. False.
: Whether a surgical guide is necessary depends on the case-the number of implants you’re placing and the number of teeth you’re replacing. When several teeth are missing a surgical guide gives the surgeon a way to position the implant correctly based on the opposing dentition, the occlusion that we want to achieve in the final restoration and the position of the implants relative to one another and the surrounding anatomic structures.
10. Every implant case should be done with a 3D scan as part of the treatment planning process. False.
Dr. John D. Da Silva, American Academy of Implant Dentistry President and Vice Dean at the Harvard School of Dental Medicine: While the use of 3D scans has increased, they are not necessary in all instances. They are important when there is a question of how much bone is present and when there are structures near the surgical site you need to avoid, particularly the inferior alveolar nerve in the mandible, and to better understand the presence or absence of bone near the maxillary sinuses. In some cases where a single tooth is being replaced and we know through periapical films and a clinical examination there is sufficient bone present, a 3D scan is not necessary.
11. Implants only can be immediately loaded when splinted together in a full-arch prosthesis. False.
Dr. John D. Da Silva, American Academy of Implant Dentistry President and Vice Dean at the Harvard School of Dental Medicine: There are a host of factors to consider when immediate loading implants, including the type and density of the bone that is present, the height of bone as well as the occlusion, the arch form and the plane of occlusion. In addition, the occlusal pattern must be considered. You need to know what teeth are involved in dissclusion and lateral excursive movements and whether the implants you’re immediately loading will be part of that function. You must also consider the amount of vertical and horizontal overlap of the teeth, as well as the skeletal classification of the case being treated. Providers must have a very good understanding of occlusion and occlusal function to determine the parameters for immediate loading.
12. Occlusion for an implant crown should be the same as that of a crown on a natural tooth. False.
Dr. John D. Da Silva, American Academy of Implant Dentistry President and Vice Dean at the Harvard School of Dental Medicine: Sometimes but not always. The provider must have a very good understanding of occlusion and occlusal function to determine the parameters that factor into determining the occlusal pattern an individual implant crown should have. It depends on the occlusion in the individual being treated and the factors found in that case. The implant does not move relative to the amount of physiologic movement there is in natural teeth.
13. Socket preservation has no effect on the eventual success of an implant and its prosthesis. False.
Dr. John D. Da Silva, American Academy of Implant Dentistry President and Vice Dean at the Harvard School of Dental Medicine: This depends on the individual you’re treating, his or her overall health, how many teeth you’re extracting and their proximity to one another. The more teeth next to one another that have been or need to be extracted, the greater the amount of resorption there will be. Socket preservation make implant placement easier, but that does not mean all sockets need preservation. Some can have implants placed immediately and others require grafting and must wait for healing before implant placement.
Related reading: How to extract teeth as atraumatically as possible
Continue to Page 7 to further test your implant IQ ...
14. GPs don't really need much training to begin placing implants in their practices. False.

Scott B. Henkel, CDT, Implant Direct Vice President of Global Education & Digital Platform: Implant placement introduces a surgical element into a general practice, and that new level of invasiveness requires proper training to ensure patient safety.
Implant therapy has progressed to a point that makes it possible for most GPs to learn the core principles and clinical skills necessary for single-tooth replacement. Understanding surgical implant placement should be affordable and accessible. The key to success is ongoing support and a guide-by-the-side mentor program - one that introduces more convenient and affordable products or services that can transform GPs into implantologists over time.
Most implant companies offer courses but haven’t changed their existing model to truly help doctors adopt implants. Implant Direct’s focus on educating GPs through an ID Passport allows clinicians to build competence and confidence affordably yet effectively over time. If you start simply and gradually but stay on course, you will eventually transform your practice.
15. Mini implants are equivalent to larger root form implants in reliability and functionality. False.
Dr. Jim Rutkowski: Mini implants have a much higher failure rate. The technology in placing mini implants is considered simpler because you don’t have to lay a flap. When you do it blindly or flapless it’s very difficult to know just where you are in placing the implant, unless you’re using a guided surgical procedure. I actually think it’s more difficult to place an implant with a flapless technique. Also the amount of surface area a mini implant has available for osseointegration is much smaller than that of a large diameter implant.
Long-term success rates show traditional implants have a much longer life than mini implants. With that said, mini implants are great as a transitional implant. They can be loaded immediately and placed between implants to give them time for osseointegration. That’s a wonderful idea. They’re also a good option for senior patients who have a known limited life span. It’s acceptable to use mini implants in these cases because you can keep them comfortable in the final stages of life.
Q&A: Dr. Joseph Gian-Grasso on trends and advances in dental implants