How to make anesthesia less of a pain
There's no way around the need to constantly deliver local anesthetics in dental practices, but there are ways to reduce the pain and fear patients feel, as well as reduce the stress of the clinician.

In DPR’s latest exclusive survey, we tackle the topic of local anesthetics, a necessity in dentistry for more than 100 years. while the needles you’ve been using have been scaring patients for just as long, there are a number of products and methods available today to make the process a lot less painful for everyone involved.
To some patients, the thought of needing dental work is disappointing enough, but the worst part is knowing that the work probably involves a date with the needle. No one likes to get dental anesthesia, but there are advances made every year that can make the experience a little less unpleasant. And dentists have a number of options to make dental work as painless as possible.
In Fall 2015, Dental Products Report commissioned a survey of dentists and hygienists about their opinions and use of anesthetics. The survey included 400 respondents, most of which (75 percent) were general practitioners. Six percent were hygienists, with specialists (periodontists, endodontists, and so forth) accounting for the remainder.
Trending article: Is dental anesthesia destroying children's teeth?
Anesthetics
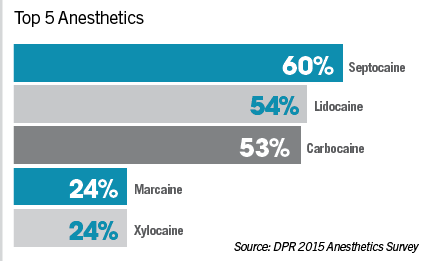
Respondents indicated that they to used multiple types of anesthetics – 35 percent used four or more while most (40 percent) used at least three. According to survey respondents, the top five anesthetics used are:
• Septocaine – 60%
• Lidocaine – 54%
• Carbocaine – 53%
• Marcaine – 24%
• Xylocaine – 24%
“Lidocaine is one that has been around the longest,” says Dr. Stanley Malamed, Professor of Anesthesia and Medicine at the University of Southern California in Los Angeles. “It’s been around since 1948. It is the standard of comparison. So whenever a new drug is introduced on the market, how does it compare to Lidocaine?”
Articaine (which is the active ingredient in Septocaine) is a relative newcomer to the world of dental anesthesia. In initial studies it performed equally as well as Lidocaine. While it is more popular in Canada (where it was introduced in 1985) than the United States (where it was approved for use in 2000), it seems to be gaining in acceptance for its overall efficacy and especially in special cases.
“Articaine is a drug that is probably the preferred local anesthetic in pediatrics and in lighter-weight patients,” says Dr. Malamed. “It’s a preferred local anesthetic if the patient is pregnant or is nursing. Articaine also works better than any other local anesthetic by infiltration in the adult mandible. The big problem with the adult mandible is that the bone is so thick that other local anesthetics, if you infiltrate, don’t work. And that’s why doctors are forced to do the inferior alveolar nerve block, which is a very frustrating injection. Articaine has a very high success rate when used by infiltration in the mandible, so there are some definite advantages to the drug.”
Continue to page two for more...
Choice
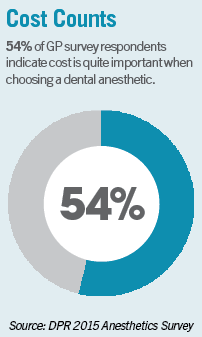
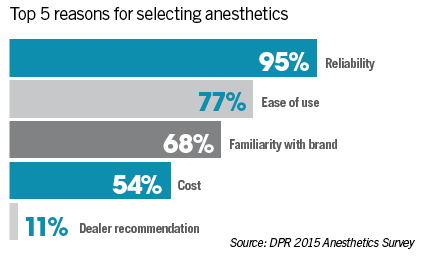
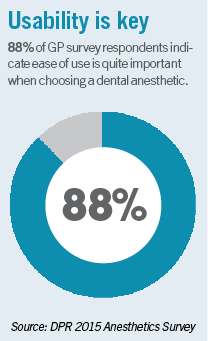
Dentists were asked what reasons they use when selecting an anesthetic. The top reasons given were:
• Reliability – 95%
• Ease of use – 77%
• Familiarity with brand – 68%
• Cost – 54%
• Dealer recommendation – 11%
Which anesthetic to use ultimately comes down to a decision based on both the patient and the procedure.
“If I’m going to do one filling on somebody and I have to get them numb, I’m going to use an anesthetic with a shorter duration of action,” says Dr. John Flucke, Chief Dental Editor and Technology Editor for DPR. “There’s no sense in getting somebody numb for three hours if I only need them numb for 20 minutes. So I will try to use something that only lasts for an hour or 90 minutes max, as opposed to using a three-hour anesthetic. Also, if I am doing something I know that I’m going to need them numb for a while, if I’m doing something like a root canal, and I want them for a while afterwards, that completely changes the regimen. I’d probably use multiple anesthetics in that particular situation.”
“It is a per-patient decision,” says Dr. John Comisi, DDS, President and CEO of Dental Care With a Difference in Ithaca, N.Y. “Most practitioners will typically have a 1:100,000 epinephrine type of Lidocaine in their practices. That’s probably the workhorse of most dental offices, and that’ll typically last about an hour, maybe an hour and a half.”
Trending article: New research discovers way to eliminate needles for dental anesthetic
The patient’s medical history also has an impact on which anesthetic is used. For instance, patients with heart problems might not be good candidates for epinephrine cocktails.
“What I consider is the health of the patient and the age of the patient,” says Dr. Sheri Doniger, DDS, President, American Association of Women Dentists and practitioner in Lincolnwood, Ill. “Certain patients have cardiac issues, and I wouldn’t want to use anything with epinephrine in it, so I make sure that the anesthetic doesn’t have epinephrine.”
“Depending on the medical history of the patient,” says Dr. Comisi. “That’ll help to determine what type of anesthetic that you’re going to use, and also how effective it’s going to be. But the most important thing nowadays is making sure that health history is understood, selecting the right anesthetic based on that, and to use a buffering agent if that is something you use in your practice, and to use any type of device or mechanism that is distracting to the patients that will help them feel more at ease.”
While Lidocaine is the most prevalently used anesthetic in the United States, procedures requiring longer anesthesia will use different agents.
“For longer, more detailed or involved procedures, you’ll want a longer-acting type of anesthetic, and that’s where you’re going to go to some of the other types that are available like Marcaine,” says Dr. Comisi. “That’s typically what oral surgeons will use for long term anesthetic effect. It’s very, very profound. Some offices, like myself, will use things like Septocaine by Septodont. It’s a very nice anesthetic. The Articaine derivative found in Septocaine provides a really good, profound anesthesia. It’s better than just Lidocaine, itself, and, typically, because it does it better than Lidocaine, you don’t have to give as much of the anesthetic.”
Continue to page three for more...
Computer control
For more than a century, the needle and syringe have been – and continue to be – the go-to means of getting patients numb. And for more than a century, patients have dreaded it. In the past decade and a half, however, some tools have helped take the sting out of injections. Computer-Controlled Local Anesthetic Delivery (CCLAD) systems manage how fast anesthetic is injected, reducing patient pain.
The original, a product of Milestone Scientific, was called the STA Wand and it has undergone several iterations since introduced in the 1990s. Currently, it is just called The Wand, and available from Aseptico, Inc.
“It’s a device that allows the dentist to deliver local anesthetics virtually painlessly,” says Dr. Malamed. “Giving injections on the palate is normally considered by the patient to be the worst, and also by the doctor the worst. They don’t like giving injections in the palate because patients hate getting them. You can give palatal injections, I’m not going to say painlessly, because that’s pushing a little bit, but you can give them virtually painlessly with a device such as The Wand, which the computer controls the delivery and the pressure of the anesthetic going in.”
Dr. Flucke notes that there are three sources of pain for an anesthetic injection:
• The initial needle stick
• The anesthetic’s pH
• The pressure of the liquid entering tissue
Trending article: Study finds home care of children crucial after oral sedation
Devices like The Wand ameliorate pain by managing the amount of pressure used to administer anesthetic.
“What the device does is as it injects, it figures out what’s the minimum pressure that I can apply to the stopper that makes it move” says Dr. Flucke. “It injects at the minimal pressure and it lets that anesthetic solution slowly defuse out into the tissues so that you don’t get a lot of pressure built up from the injection.”
Dr. Flucke didn’t think highly of The Wand when he first encountered it, but has come to appreciate it.
“When I first saw it, I thought, ‘This is the biggest placebo I’ve ever seen in my life,’ ” says Dr. Flucke. “Of course it beeps and dings when you’re using it. It’s got LEDs. It’s a great distraction. You tell patients, ‘Oh, you’re not going to feel a thing because it beeps and dings and has LEDs.’ As I was using it, more and more people said, ‘You know what? I think that’s better.’ ”
Dr. Flucke’s “a-ha” moment came when a patient specifically asked for it.
“The turning point came with one patient,” remembers Dr. Flucke. “He sat down; I loaded the cartridge in the syringe; and the guy looked over at me, sees the syringe in my hand, and says, ‘Where is the dingy thing?’ I’ll never forget that. He called it the ‘dingy thing.’ I said, ‘It’s next door.’ He said, ‘Well, I don’t want you getting me numb without that dingy thing.’ ”
Dr. Flucke continues, “That was the big moment. The shaft of light came down from on high and I heard choirs sing, and I thought, ‘There’s something to this.’ Even if it’s a giant placebo, people want it. People are now requesting it. From that point on, it became a standard part of what I do.”
Continue to page four for more...
Reversal
Patients need to get numb, but there is also value in getting un-numb. After a procedure, some patients may go hours unable to feel their mouths. A product called OraVerse, from Septodont, reverses anesthesia.
“Let’s say you’re a businessperson giving an interview to Dental Products Report, and your lip and tongue are still numb,” illustrates Dr. Malamed. “It would be kind of hard to speak. If I was going to a big dinner or something and your mouth is numb, it makes it hurt to eat. OraVerse is a vasodilator. It counteracts the effect of the epinephrine. At the end of the dental procedure, when you finish cutting on the tooth, you inject it back into the same area you put the local anesthetic previously. Using a vasodilator increases blood flow to the area, so the anesthetic is taken away from the area faster, and the soft tissue anesthesia decreases dramatically – by several hours in most cases.”
“It basically helps to reduce the time the patient is numb post-procedure,” says Dr. Comisi. “It’s a special reversal agent that is a nice adjunct to have at the office, because you have business people that sometimes have to go back to the office, they have a meeting, they don’t want to have that sloppy lip flopping around. Having OraVerse in the office you can just say, ‘Hey listen, I can do the procedure, get finished, and then I can give you another injection that will reverse the anesthetic so you won’t be numb when you get back.’ Some patients like that idea. You have to deliver the same amount of OraVerse as to how much anesthetic that you injected, so if you inject one carpule anesthetic you have to inject one carpule of the OraVerse to enable that reversal of anesthetic to occur.
Trending article: Do men require more sedative than women during oral surgery?
But reversal agents are not widely used for a couple of reasons, the first being patient preference.
“I don’t use it as much, because patients are more willing to just allow things to wear off,” says Dr. Comisi. “But in those situations where I have a critical circumstance, when the patient has to get back to a big meeting and they don’t want to have that feeling, it’s been nice to have it on hand.”
Some dentists may not even offer it, because they don’t see the immediate benefit for themselves.
“(To some dentists) it has limited use,” says Dr. Malamed. “It has not done well for a very simple reason: The first thing that dentists ask is, ‘How much is it going to cost?’ And the answer is always, ‘Well that’s too much.’ The problem with OraVerse – and it’s not a problem with OraVerse, it’s a problem with dentists’ mentality towards it – let’s say a cartridge costs five or six dollars. The dentist injects it at the end of the procedure and then sends the patient home. So from the dentist’s perspective, they don’t see a benefit from that product. The patient sees the benefit. It’s a quality of life product. The patient leaves the office and gets un-numb. The sensation comes back faster and they continue in their life more normally. Sadly, and for a lot of dentists out there, ‘If I don’t see the benefit of it, I don’t want to use it. Six dollars a cartridge is too much money for this.’ Which is sad, because it’s a really good product.”
Continue to page five for more...
Buffering agents
Doctors don’t have to rely on anesthetics alone to help get patients numb. Buffering agents are adjuncts that can help speed up and deepen the anesthetic effect.
The buffering agent helps in two ways: First, anesthetics have a low pH cause pain because they have a higher level of acidity than tissue. Also, lower pH solutions contain anesthetic in a freely diffusible form, which leads to a longer time for anesthesia to set in. Once mixed with a buffering agent, anesthetic works its way into tissue faster and is less painful.
“Local anesthetics are very acidic, and when you inject the local anesthetic into the patient’s mouth, it burns,” says Dr. Malamed. “The onset of anesthesia is a little bit slower, so what we do is we raise the pH. We’re adding something called sodium bicarbonate to the cartridge – a very small amount of sodium bicarbonate. You’re raising the pH from 3.52 about 7.35, and what that does is it’s no longer acidic, so it no longer burns on injection. It also dramatically speeds up the onset of anesthesia.”
Dr. Malamed notes that a study of mandibular blocks with Lidocaine and the onset of pulpal anesthesia showed the un-buffered Lidocaine achieved anesthesia in six minutes 51 seconds, while the buffered Lidocaine only took one minute 51 seconds.
“It was a dramatic difference,” says Dr. Malamed.
Trending article: Tips and tricks on digital photography for case presentation
Onpharma Inc., introduced the first buffering system called Onset. This is now distributed by Orapharma, Inc. It is a three-part system: the Onset mixing pen, cartridge connector, and a sodium bicarbonate injection solution. The solution is an 8.4 USP neutralizing additive solution. When combined with a 1.8 mL cartridge of local anesthetic, patients experience a faster, more profound numbing effect.
Anutra Medical offers a buffering system with a different delivery system. Rather than snap the carpule into an injector for a one-time use, the Anutra Dispenser allows multiple doses of sodium bicarbonate and Lidocaine. Once loaded into the dispenser, the dentist selects how much he or she wants and then draws is from the dispenser with a disposable syringe.
“Both of these items are very interesting, because the whole difficulty with some types of anesthetic effect is that the acidity of the anesthetic and the acidity of the injection site would delay the overall effectiveness of a local anesthetic,” says Dr. Comisi. “So that would be problematic, but with something like these buffering solutions that can be added to the anesthetic solution, anesthetic can be effective in a matter of moments rather than in tens of minutes. That is one of the things that we have incorporated into our practice which makes, procedurally, our overall activity with a patient quicker, easier, and a more profound anesthetic effect.”
While buffering agents seem to offer benefits to dentists, not everyone is sold on their necessity.
“If I have somebody that I attempt to get numb, and if I give them an injection, and I have to wait five minutes to go to work, it’s not that big of a deal for me,” says Dr. Flucke. “If I use the buffered anesthetic, I could go to work in two minutes. I do understand the logic of that, but my biggest thing is that I don’t know what I would do with that extra short time span. Sometimes there are times when I just need to take a break. I just need to step away from dentistry in general and get my wits about me. I feel like it makes me a better clinician to give myself a second. There’s a reason why every professional sports league allows timeouts. Sometimes you just need to regroup or take a breather, and I sort of look at anesthesia time as my timeout.” Dr. Comisi however states, “I find that it expedites the procedures I provide to my patients and gets even the “hottest” most painful tooth prior to endodontics, become numb, faster and better. That to me makes buffering invaluable.”
“This is a product that is doing very well for simple reason: the dentist sees the benefit,” says Dr. Malamed. “The OraVerse is a great product that is not doing do that well, because the dentist doesn’t see any benefit, the patient does. The dentist sees all the benefits to this Onset product.”
Continue to page six for more...
Good vibrations
Another type of tool used too mitigate pain involves what’s known as “Gate Control Theory.” The idea being that a vibration sensation in the mouth reaches the brain before a pain signal. As such, vibrating the area around the injection site can distract the patient from sensing pain.
There are two devices on the market that operate on this theory: The DentalVibe injection comfort system and the VibraJect, which is distributed in the United States by Golden Dental Solutions.
A full line of dental anesthetics is available through Henry Schein.

The VibraJect is a small vibrating device that attaches to a conventional syringe, providing the vibrations. The DentalVibe is a separate device with disposable tips that is used in conjunction with the syringe.
Related reading: 4 products that make the discomfort difference for dental patients
“The DentalVibe looks like a Sonicare toothbrush,” says Dr. Flucke. “Instead of toothbrush bristles, it has a Y on the end. The idea is you take this device and turn it on and it vibrates at a very high rate. You put the Y against the tissue and you inject between the arms of the Y. It shakes the tissue for you and it oscillates at the proper rate for the most painless type of injection.”
Dr. Comisi also favors the DentalVibe.
“That also has been very helpful in masking the injection site,” says Dr. Comisi. “It’s a very nice device. It’s gone through several incarnations, each improving the mechanism, and it’s a nice way to use a conventional syringe and provide an anesthetic that patients don’t have to be as anxious about receiving. It’s a nice adjunct. In my hands it’s been very useful.”
Continue to page seven for more...
High anxiety
Dentists have, for years, pumped Muzak or other smooth, relaxing music into their operatories to calm nerves. Advancing on that practice, some doctors allow patients to bring in their own music. Dr. Comisi sanctions that and offers some other comforts, as well.
“If patients want to bring in headphones they’re welcome to bring them in and listen to their specific music while we’re working,” says Dr. Comisi. “We have a feature on our chairs that is a massage feature and gives a little bit of heat to the back as well. Our patients like to sit in our chair or turn on the massage feature and just relax. We offer them nice and comfortable pillows to put behind the small of their back or behind their head.”
“Telling a lot of bad jokes doesn’t help,” he adds. “And I’m notorious for bad jokes.”
Related reading: Cognitive behavioral therapy found to help dental phobias
Dr. Doniger has a somewhat unorthodox way to ease patient anxiety.
“I give them rocks,” she says. “I literally give them beach rocks that I have selected over the course of the last several years. People hold on to them. I also explain the procedure step-by-step. The biggest fear is fear of the unknown, so I will say, ‘Do you want to hold onto a rock?’ And they say, ‘Really? A rock?’ And we say, ‘Yeah, it’s a real rock.’
In conjunction with the beach rocks, Dr. Doniger utilizes other techniques to help soothe patients.
“We have a rock library, they hang on to the rock, and then I tell them what I’m doing,” she says. “I put the topical on and I leave the topical on for at least a minute and a half, and we talk – we just talk about everything – and then I tell them what I’m going to do, and that it may pinch a little bit. I make sure that they’re breathing, because breathing is important. I tell them that I’m not a pathologist. I don’t want to work on dead people. So a little bit of humor, a little bit of cajoling, and – for the most part – the biggest thing is to make sure that they’re breathing, because it’s easier to give anesthetic when the tissue is relaxed, and if somebody is holding their breath, their tissues aren’t relaxed."
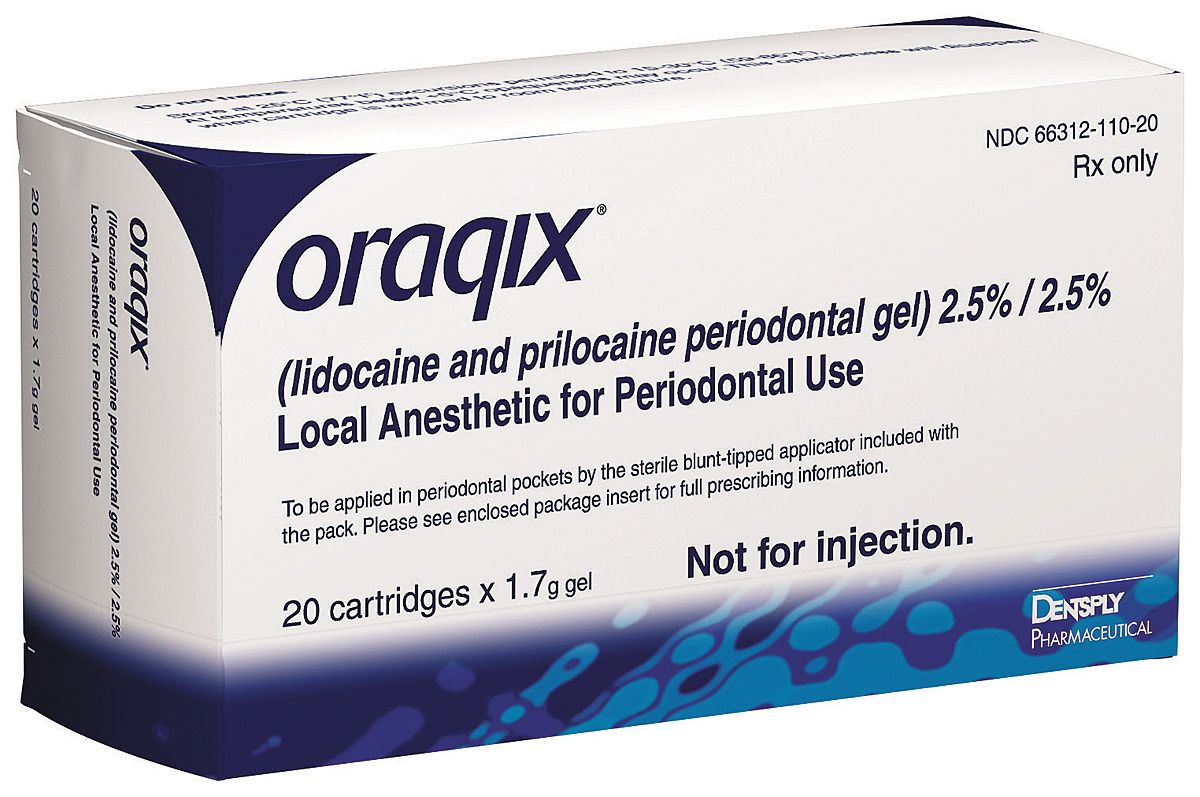
Oraqix lidocaine and prilocaine periondontal gel offers patients pain relief.
Dr. Flucke has monitors mounted over each chair in his operatory so patients can watch television or movies. He also has a Netflix account for the office so that patients can watch whatever is available.
“The nice thing about that is if somebody comes in and you got cable, for instance, they want to watch TV show and they get started at 3:15, the show started at 3:00,” says Dr. Flucke. “So if they want to watch some show, they’re getting into it 15 minutes late, but with Netflix it just starts whenever you click play.”
The key to managing patient anxiety is calming them down.
“The magic thing to do is sedate them,” says Dr. Malamed. “Sedation doesn’t automatically imply using drugs. Sedation is all about distracting the patient; take the patient’s mind off of what you’re doing. The scared patient is sitting in the dental chair and is overly alert to everything that is going on. They don’t want to be snuck up on. They watch the instruments. They just overreact. We’re trying to slow them down. A really scared patient, if you blow air toward their mouth, they’re going to go, ‘Ow!’ And even though that really can’t be painful, they’re waiting for anything to hurt. The sound of the handpiece. The touch of your hand. They over-respond. They’re not feeling pain, but psychologically they’re feeling pain, and that hurts just as much as real pain. Take your patient’s mind off of what you’re doing by using sedation.”
Related reading: 3 easy ways to calm dental anxiety
A simple technique is simply listening and communicating with your patients.
“Sometimes patients are so wound up because of other extraneous things, that all we do is talk, and the gratitude by the patient for us just sitting and listening to them and being a good listener really helps them a lot,” says Dr. Comisi. “It has nothing to do the procedure, but sometimes you’ve just got to talk to help them get comfortable with who you are and what you’re doing.”
Continue to page eight for more...
Inhalation sedation
A method of sedation that gets somewhat mixed opinions from doctors is the use of nitrous oxide.
“Dentists seem to fall into two camps with regards to nitrous: They either love nitrous and think it’s a wonderful adjunct; or they hate it and they think it’s a tremendous hassle and it’s not worth it,” says Dr. Flucke. “I like it and I happen to think it works well and it’s a nice thing to have on hand. But I will also say that I am very much a patient-friendly doctor, and, to me, if it improves the patient experience, then it’s better for them and it’s better for me. I can work more efficiently, and that’s huge for me. If I can work more efficiently, then I can get the procedure done quicker.”
But not every doctor embraces nitrous.
“I don’t believe in nitrous,” says Dr. Doniger. “I believe that we have built a very interesting practice on patients that have been fearful of the dentist, and, of course, one of the biggest fears is the anesthetic.”
Nitrous remains a popular method of sedation and one that dentists – whether they want to use it or not – are required to learn how to use.
Related reading: Nitrous oxide: What dental professionals need to know
“My philosophy has always been that nitrous oxide oxygen is absolutely the number one technique to use,” says Dr. Malamed. “It’s something that since the 1980s the Council on Dental Accreditation (CODA) has mandated that you have to graduate dental school proficient in the use of inhalation sedation with the use of nitrous oxide, and yet the percentage of general dentists using nitrous in the United States has remained about 35 percent. Even though, within specialties like pediatrics, most pediatric dentists use nitrous and virtually every oral surgeon uses it in conjunction with other techniques. So it’s out there. It’s a great technique. That should be the starter technique for using sedation and dentistry.”
In building his new dental office, Dr. Flucke even constructed it with infrastructure for nitrous.
“I would highly recommend for people to plumb for nitrous,” says Dr. Flucke. “There are two ways to deliver nitrous in dentistry: You can either run actual copper pipes to your treatment areas, or there are little portable systems, carts, that you can wheel around. It’s less money to set up, but in the long run the cart system costs you more money – you run out of nitrous, frequently the bottles on those cards are a hassle. So I recommend to doctors that you plumb for it. It will cost you more out-of-pocket initially, but you’ll be thrilled that you did it in the long run.”
Continue to page nine for more...
Best results
Achieving the best results in anesthesia involves an amalgamation of all these philosophies and techniques that depend on both patient needs and the clinician’s style.
“I think it’s not so much of what’s new with anesthesia as I think it’s the technique,” says Dr. Doniger. “I think what’s new is really old. The biggest part about what’s new with anesthesia is the clinician truly taking their time to give a proper anesthetic. A lot of times people are worried about the bottom line and they want to get the anesthetic in as quickly as possible and start to work before it’s actually ready, so you have to have a very good topical anesthetic, and you use it the way the instructions told you to use it – dry off the tissue and let it sit there for a period of time, because if you put it on and just touch the tissue, it’s not going to give much anesthetic, and you really don’t get numb from that. Again what’s new is old – going slow.”
“The biggest thing with the anesthetic is people tend to go very fast because people hate the anesthetic needle in their mouth, so in reaction to that, people tend to go a lot faster, where they shouldn’t,” says Dr. Doniger. “Because what we’re doing is we are taking liquid and putting it in an area that was very happy living by itself without having this additional liquid pushing away tissue in there. When people are stressed and they’re really clenching their mouths, it’s often difficult given that you have to make sure that they’re relaxed because – just as if you made a really hard fist I try to poke you with my finger on your bicep, I wouldn’t be able to budge it. But if your arm is relaxed, and I take my finger and I touch your bicep, I’ll be able to move it. I take my time when I give my anesthetic. I don’t pound it all in. I don’t pump it all in in one second. I make sure that it’s going like a couple millimeters at a time and that’s it. However long it takes. I am in no rush when I’m giving anesthetic. There is nothing that I would rather do at that moment in my life than give anesthetic, because that’s my main focus. I’m not going to be thinking about what I’m doing next or the next patient, or a phone call I have to return. That’s the focus.”
Trending article: 10 ways to make a great impression
Buffering agents and other tools to help reduce pain and anxiety will help.
“In today’s busy practices, a buffering agent solution is certainly essential, because it will help to get the anesthetic effect quicker,” says Dr. Comisi. “That’s a huge asset to have in the office. To have something like the DentalVibe can also be helpful. The cost for these items is not remotely challenging for most dental offices.”
Dr. Malamed observes that Articaine delivers very good results and can help even if the perfect injection site is missed.
“Articaine, even if you miss the block, you can then do it by infiltration in the mandible and you have a very good chance of getting anesthesia,” says Dr. Malamed.
And while there are a number of anesthetics out there, a lot of their effectiveness comes down to good technique. “They’re all good drugs,” says Dr. Malamed. “If you deposit a local anesthetic close enough to the nerve it is going to block nerve conduction, and that’s the problem. Because every injection we give in the human body, once the needle penetrates that mucous membrane in the mouth or the skin, every injection is blind, and we can’t see the nerve we’re aiming for. The biggest problem we have in dentistry is in the mandible, because that inferior alveolar block is very elusive, it’s very hard to find sometimes.”
Delivering anesthetics has been largely the same for more than a century, but recent advances in agents, methods, and techniques to deliver those anesthetics have made the patients’ – and doctors’ – dental experiences more pain-free.